By Catherine Carr
If you live in America today, you might have noticed a mental health epidemic unfolding. While debate rages over the cause of the decades-long upswing in depression, anxiety, and PTSD, one thing is clear: most of us know at least one person who has been, at some point, dangerously depressed. Worse still, we probably all know someone whose depression has not responded to first-line medications like SSRIs.
Watching our neighbors and loved ones struggling with deep depression can raise existential questions. And indeed, many researchers are asking what we are doing wrong as a society to have so many of our people in these dire straits. Yet, another avenue of research is drawing on the wisdom of previous decades and millennia to treat these seemingly un-treatable conditions.
Plant medicines, including psychoactive compounds, have been used for millennia by indigenous peoples to produce profound changes and healing in their users. In the mid-20th century, a wave of Western academics suggested that newly synthesized hallucinogens could also have profound therapeutic benefits. However, a wave of government crackdowns in the late 20th century made it illegal for even research scientists to possess or administer any hallucinogens, including the plant medicines of indigenous peoples, before definitive results could be found.
The first decades of the 21st century have seen a loosening of these bans, and a subsequent explosion in clinical research into plant medicines and synthetic psychedelics. The results have been astonishing. Medical and recreational marijuana has been legalized across swaths of America with astonishing speed, and early studies of the use of ketamine and psilocybin under the supervision of trained therapists have shown such strong results that both medicines have already been approved for compassionate use for patients in some countries when other treatments have failed.
One of the more remarkable aspects of this research has been the finding that a substantial portion of patients who experience remission of their treatment-resistant depression after using these medicines also have religious experiences during treatment. This has forced some clinicians who make use of them to begin learning about traditional shamanistic and other compatible theologies to help their patients make sense of their experiences.
In this article we’ll briefly discuss the state of research into several ancient and modern medicines whose abilities to open the mind are now being studied by doctors and scientists.
Marijuana
Once demonized as the cause of “reefer madness,” mountains of clinical data have finally convinced politicians that marijuana is no more dangerous than alcohol or tobacco—and has much more medicinal value than either of those long-accepted recreational drugs. Between THC, CBD, and thousands of other unique bioactive compounds, medical marijuana can now be prescribed in many states for the treatment of anything from life-threatening intractable seizures to anxiety and chronic pain.
Doctors caution that inhaling smoke is bad for the lungs no matter what is in the smoke, and that the use of psychoactive compounds in pregnant women and children under the age of 18 should be restricted to medically necessary uses because all psychoactive compounds can affect the development of growing brains in detrimental ways.
Far from being the demon it was once regarded, marijuana is now viewed by many patients and doctors alike as a near-miraculous medicine for hundreds of painful and dangerous conditions. Its recreational use is also now considered on par with the use of recreational alcohol in many states.
Psilocybin
Long touted as “magic mushrooms,” the many fungi species that produce the compound psilocybin have been used by shamans and psychedelic adventurers alike. Many users have reported profound, life-changing religious experiences—but the potential for life-changing negative experiences including psychotic episodes, suicidal ideation, and seizures have caused shamans and medical doctors alike to advise against the use of these mushrooms by patients who are not spiritually prepared and supervised by trained experts.
Many people who have used psilocybin agree with this assessment. One person, who spoke on condition of anonymity, described her first trip as a bad one. “I felt so incredibly abandoned,” she says, speaking of being left alone by her friends for a few minutes while under the influence of psilocybin. “It was like being a newborn baby and having your mom, who you depend on for life, abandon you. I was in this state where anything seemed possible. And when they left, part of me was like—what if I died? What would happen? I became really curious about that. I thought seriously about the knives in the kitchen. If I’d had better motor control at the time, it could have been very bad.”
But she also reports enlightening experiences with the mushroom when working with a skilled trip sitter. “It’s like being born again,” she said. “And that can be amazing and enlightening, or it can be traumatizing, depending on what’s going on. I was seeing things in a way I’d never seen them before. It was like I was seeing and feeling everything for the first time. I was experiencing things I hadn’t known I could experience. If you’re confined in a closed space and you’re alone, and you feel like you just came into the world and that’s what the world is, it can be the most terrible experience. But if you’re surrounded by beauty and you’re outdoors with someone watching over you, it can leave you with this amazing sense of beauty and awe of life. You experience things you never thought were possible, and you get curious about what else is possible. But if you start wondering what life after death is like, for example, and you’re left alone and unsupervised, it can be very dangerous.”
Results of recent studies have echoed the millennia-old wisdom of the shamans: the effects of psilocybin appear to be mostly beneficial as long as patients undergo proper mental preparation in advance and are overseen by experienced healers while taking the mushrooms. Clinical trials have also found better safety results from excluding patients with family histories of schizophrenia and psychotic disorders from their studies, as the mushrooms seem to trigger latent disease mechanisms in some people with genetic predispositions to those illnesses.
Early studies of psilocybin’s therapeutic effectiveness for treatment-resistant depression and PTSD have gone well enough that the drugs have been approved for compassionate use in a handful of patients. With dozens of clinical trials of psilocybin’s safety and effectiveness set to be completed in the next decade, we’ll soon know more about the reliability and safety of these magic mushrooms.
Mescaline, Peyote, and San Pedro
Mescaline is the main psychoactive ingredient in many plant medicines used for religious experiences in the Americas. The peyote used by the Native American Church under religious freedom laws, and the San Pedro plant used by South American shamans, both feature mescaline among the major players in their psychoactive effects.
For the Native American Church, the sacramental use of peyote with proper training and preparation is intended to heal mental, physical, spiritual, and social ills. The Native American Church has been able to obtain religious exemptions for the sacramental use of this plant despite it being considered among the most highly illegal substances to possess or distribute in the United States today. To the shamans of the Andes Mountains, ceremonial use of the San Pedro cactus has been used to treat both physical and spiritual ills, with its name, translating to “St. Peter,” deriving from the belief that the plant, like St. Peter in Christian theology, holds the keys to Heaven. The Western medical community has considered mescaline for the treatment of addiction and mental illnesses involving serotonin deficiencies, though its use for these applications in the absence of training and guidance from indigenous practitioners has so far yielded a mix of helpful and harmful results.
Mescaline presents a fascinating case in which spiritual preparation really does make a difference to the outcome from using plant medicines. While the profoundly beneficial experiences reported by America’s First Nations led to a frenzy of medical interest in mescaline, peyote, and San Pedro in the 20th century, preliminary results puzzled scientists. Just like with psilocybin, the reactions of unprepared modern Westerners to these plants could be negative or neutral as often as they were positive. The “disconcerting unpredictability” of the plants’ effects, which included intensely uncomfortable paranoia and potentially dangerous physical side effects in early test subjects, caused research into the therapeutic potential of mescaline to grind to a halt. But why should First Nations people experience a drug differently from modern Westerners?
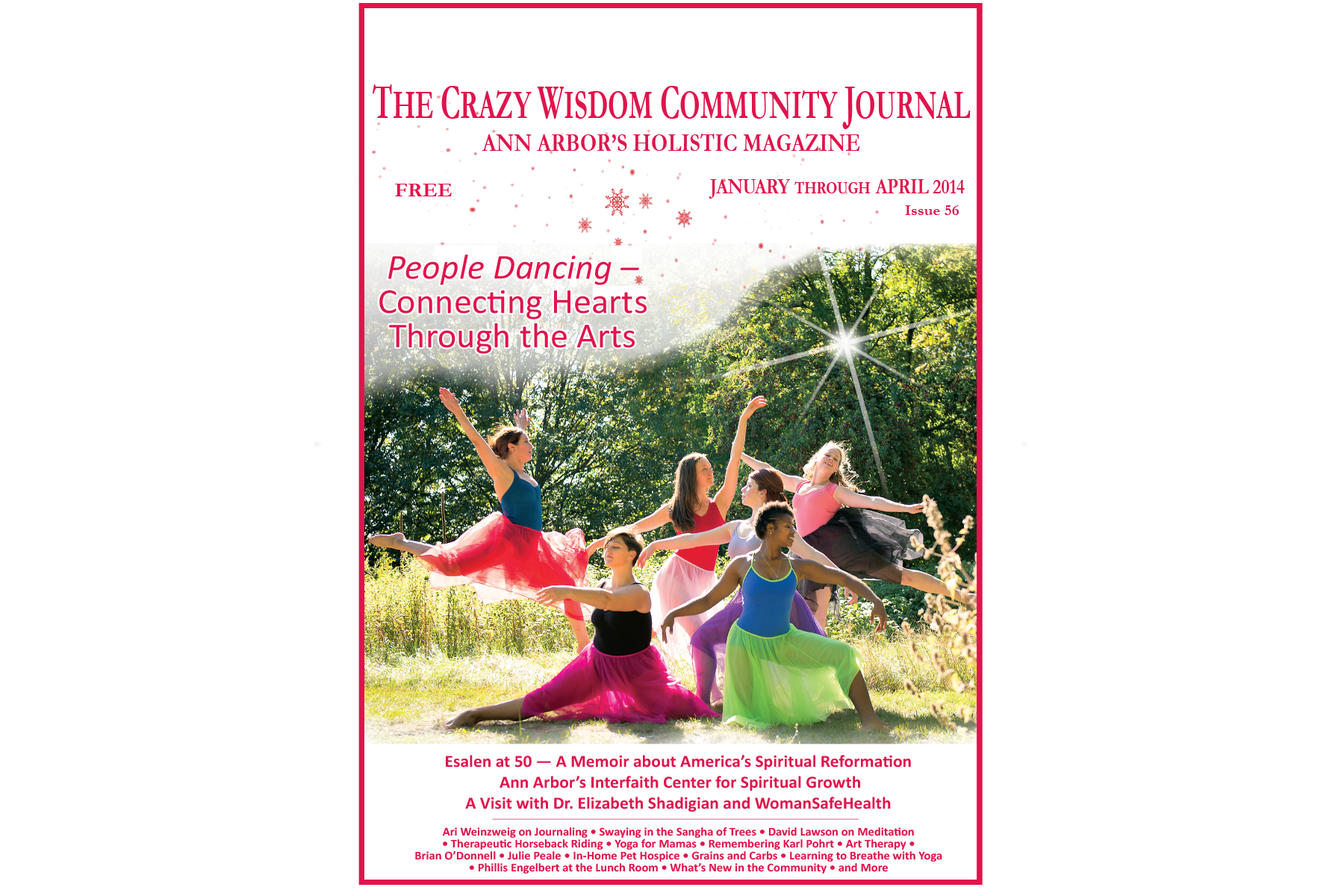
Read related article: Esalen at 50: A Memoir about America's Spiritual Reformation
This outcome is not so surprising when one considers that psychoactive medications work through the method of juicing up existing neural networks. Because many of our brain’s neural networks are built by learning, memory, action, practice, and emotion, it makes sense that people who have certain cultural practices and beliefs would have different neural networks from those who do not. First Nations people raised with cultural practices in symbiosis with mescaline-bearing plants, and who were raised to revere and have positive expectations of these plants from an early age, may well be predisposed to activate certain sacred neural pathways that secular Westerners may simply never have developed when they take mescaline.
Does this mean that only people born into First Nations cultures can enjoy the benefits of mescaline? Probably not—anecdotal evidence suggests that the simple psychosocial preparation granted by participating in Native American Church services may be sufficient to get good results. But people who are not receiving guidance from qualified First Nations practitioners may not be able to use these medicines with the expectation of safety.
It is unclear precisely which practices are needed, or how long they must be practiced, to develop the neural networks that make a great experience of mescaline more likely. Many variables, including what teachings a person has received, what expectations they have built up, and the behavior of the people around them, may affect which neural networks activate in response to mescaline.
So, on this one, it may be a good idea to listen to the First Nations practitioners who have used these plants for millennia. They generally advise that these plants only be used under the supervision of an experienced First Nations practitioner. And the people who recommend that have proven that they know more than modern medical scientists about how precisely to prime the brain to receive therapeutic benefits from mescaline while avoiding the potential dangers of this powerful medicine.
Ayahuasca
Ayahuasca is a plant medicine whose popularity has exploded among spiritually minded people in recent years. Made from a combination of two local plants by peoples native to the Amazon River basin, ayahuasca, like the other items on this list, is recommended to be prepared and consumed only under the supervision of well-trained shamans.
When used properly, users report profound spiritual awakenings which may include new insights into the nature of reality and/or contact with spirit guides from other planes of existence. The plant medicine’s physical side effects can sometimes prove dangerous, mostly in people with pre-existing medical conditions or who have other substances or medicines that may interact negatively with ayahuasca in their bodies.
Like psilocybin, ayahuasca has shown early promise in clinical studies. The studies conducted so far have been too small to gather reliable data on this plant medicine’s safety and effectiveness, but their results have been sufficient to prompt much more research which is currently ongoing.
U.K.-based researchers working with traditional shamans at the Riosbo Ayahuasca Retreat and Research Center in Peru are investigating whether ayahuasca can safely and reliably provide therapeutic benefits including long-term improvement of trauma-related conditions, long-term reductions in anxiety, increases in openness to new experiences, and long-term improvements in symptoms of ADHD.
Intriguingly, one current avenue of research is based on preliminary evidence that ayahuasca may be able to reverse epigenetic changes which occur as a result of personal or generational trauma. Severe trauma in one’s personal or ancestral past has been shown to cause chemical changes to DNA which can result in lifelong changes to individual emotional processing, and which can even be passed on to future generations.
While the idea of inheriting ancestral trauma in a literal genetic sense may seem bleak, scientists have also discovered that these chemical changes to DNA can be reversed for oneself, and potentially future generations of one’s family, using certain practices. Practices including certain forms of psychotherapy and physical exercise have been found to reverse the changes to our genes caused by trauma. This means that practices we undertake to heal ourselves may result in lifelong changes to our DNA and may even be passed on to future children who may inherit the healed version of our DNA as a result of the work we do in our lifetimes.
Current studies are working to determine if the epigenetic healing permitted by these practices really can heal our descendants of past ancestral trauma. If this proves to be the case, ayahuasca may prove to be a way of producing lifelong epigenetic healing, not only for ourselves, but for future generations.
As these research studies are completed, we expect to learn much more about the safety and potential benefits of ayahuasca for Westerners not raised in the ayahuasca traditions in the next decade. Interested readers can donate directly to these research efforts by visiting AyahuascaFoundation.org/Research.
Ketamine
A controversial entry on this list because it is not a plant medicine, ketamine is nonetheless a psychedelic medicine that has been described by Hashimoto in a historical overview published in Psychiatry and Clinical Neurosciences as “the single most important advance in the treatment of depression in over 50 years.” Like psilocybin, ketamine often produces religious experiences and sensations of contact with the divine in patients who may subsequently experience lasting remission of previously life-threatening depression.
Originally used as an anesthetic due to its ability to blunt the sensation of physical pain, ketamine’s antidepressant action, which seems literally miraculous to some patients, was first discovered in the year 2000. Its precise mechanism of action is unknown, but some studies suggest that ketamine may actually prompt brain cells to grow new connections when introduced to the system. This may explain why its effects, unlike those of most mainstream psychiatric medications, persist long after the medication is out of the patient’s system.
Not all patients experience improvement after taking ketamine. In one clinical trial, about three out of ten patients who tried ketamine did not improve. As with the other items on this list, ketamine is authorized to be used only under the supervision of trained clinicians, due to many risks including the risk of contamination with other psychoactive substances and improper dosing from ketamine that is sold illegally.
Moving Forward
The benefits of ancient plant medicines remain woefully under-studied by Western science. The intriguing questions raised by research studies to date ask us to go deeper, questioning the role of our society’s beliefs and culture in the epidemic of mental and spiritual illness we see today. The fact that people raised in Western culture do not always enjoy the same beneficial relationships with plant medicines as the people of the cultures who grew up alongside them should give us pause as we decide what really needs to be changed in our cultures and communities in order to heal our souls.
However, early evidence indicates that some plant medicines and other psychedelics may be our friends in this healing process. The amazing performance of ketamine and early good results from psilocybin studies indicate that we can still use such medicines to access divine healing by any other name.
More research is needed into other plant medicines before we can determine what teachings, beliefs, and practices are necessary to use medicines like ayahuasca and peyote safely in Western society. Still, the tantalizing glimpses shown by these cultures, and the Western scientists who study them, hints at the joyful relationship with the divine and the natural world that may be possible for us with help and guidance from plant medicines and the peoples who use them.
Catherine Carr obtained her bachelor’s degree in neuroscience from the University of Michigan in 2011. She coordinated clinical research studies, including studies of the use of ketamine for treatment-resistant depression, for five years before becoming a full-time writer. Her studies in recent years have been focused on investigating U.S. spiritual circles and their community healing practices. She now seeks to combine the disciplines of clinical research with the wisdom of spiritual traditions in her work.





































To build your pelvic power, it is vital to de-stigmatize the pelvis and its functions. No one feels uncomfortable talking about their arm, leg, or stomach muscles. There are dozens of classes and machines at the gym for building flexibility and strength in these areas—yet none for your pelvic floor.