By Madonna Gauding • Photos by Mary Bortmas
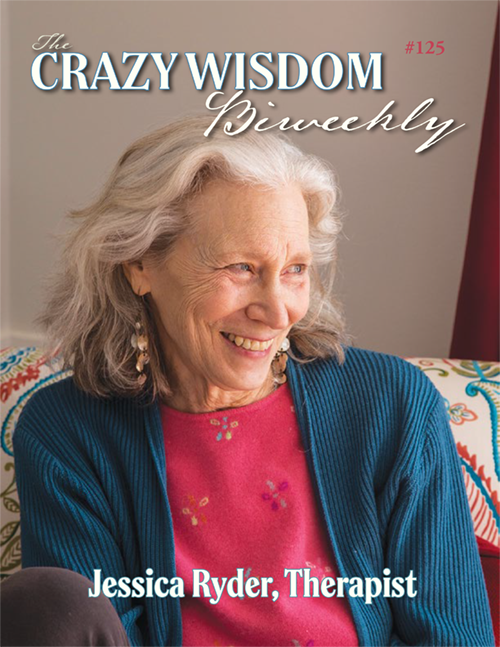
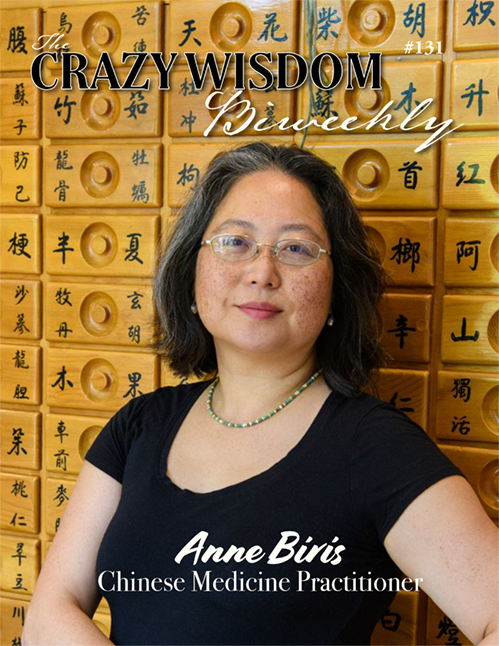
Anne Biris is a nationally board certified and State of Michigan licensed acupuncturist, Chinese herbalist, massage therapist, and practitioner of Chinese Medicine with offices in Ann Arbor and Dearborn Heights. She holds a Master’s degree in Chinese Medicine and has been practicing for 30 years. She also provides acupuncture on a volunteer basis in the poorest areas of India and Sikkim. Biris likes to fly under the radar, but after much prodding (because Anne Biris is a treasure that readers of CWCJ should know about), she agreed to sit down with me for this interview.
Madonna Gauding: So, let’s start at the beginning. Where were you born?
Anne Biris: I was born in Seoul, Korea in 1973. My name was Jin Soon Cho. I don’t know at what age I was dropped off at the orphanage. The records claim my father, a taxi driver, committed suicide leaving my mother, a housekeeper, to raise me and at least one other child on her own. In the patriarchal culture of Korea all social worth and legitimacy comes through the father. As a single mother, my mother would have been a social outcast, and I and my siblings would have been denied the advantages and opportunities of those with fathers. It is likely that financial and social pressures led my mother to relinquish me to an orphanage. There was the hope, among single mothers in Korea, that their child would be adopted by a family in the United States and have a chance at a better life.
I was four years old when my American parents, Dean and Charlotte Biris, adopted me in 1977. My first memory is arriving at Chicago’s O’Hare airport. That’s when I became Anne Biris. I have no memory of my life in the orphanage or my life in Korea. Two years later, my parents divorced, and my father moved to Wisconsin. My childhood years were spent going back and forth between Illinois and Wisconsin, sometimes living with my mother, sometimes with my dad.
Madonna Gauding: I first knew you as a patient. You read lips so well it took me several visits before I realized you were deaf. How has being deaf affected your life and your practice?
Anne Biris: Being deaf is something you are used to, like being left-handed. It does make it challenging with communication at times especially if a patient is face down on the table. But, on the whole, it causes me to pay more attention. I can’t be distracted when “listening” to my patients.
Madonna Gauding: When did you first become interested in acupuncture and Chinese medicine?
Anne Biris: I graduated a semester early from high school. Right after my last class, I left for Hawaii to visit family friends and I ended up staying for six months. While in Hawaii I met a woman acupuncturist, and I immediately knew that was what I wanted to do with my life.
MG: Why acupuncture and Chinese Medicine?
AB: Well, I knew I wanted to do something in healthcare. And in high school I had studied tai chi, Buddhism, and Asian philosophy. So, acupuncture and Traditional Chinese Medicine were a natural extension of my interests. When I returned to Wisconsin, a branch of The Chicago-based Midwest College of Oriental Medicine had just opened in Racine. I joined the first class in Racine.
MG: How old were you?
AB: I was 18 when I enrolled in acupuncture school in 1991. Technically, students were required to have completed two years of college before they enrolled, but the school made an exception and allowed me to attend community college at the same time I studied acupuncture. While attending school, I supported myself by working at the Theosophical Society in Wheaton, Illinois. In 1994, I received my certification in acupuncture and Oriental massage from the Midwest College of Oriental Medicine. In 2006, I earned a Bachelor of Science degree in Traditional Chinese Medicine Nutrition, and a Master of Science degree in Oriental Medicine from the Midwest College of Oriental Medicine.
MG: What is Chinese medicine and how is it different from standard western medicine?
AB: Chinese medicine is one of the few forms of healthcare that considers the whole person—their body, their emotions, their personal history, and everything going on with them in the moment. A good practitioner is able to incorporate every aspect of the patient into their treatment strategy. The treatment is not just choosing acupuncture points and inserting needles. It involves listening to the patient and understanding their unique needs. An individual may see five different acupuncture practitioners but will get the best results with only one, not because that person is a better acupuncturist, a better needler, but because they resonate with them on a personal and emotional level. The relationship between patient and practitioner in Chinese medicine is an integral part of the healing process.
MG: What kinds of patients do you see?
AB: I see patients of all ages, with all medical conditions, and from all walks of life. For example, I have worked with a lot of veterans who are often skeptical about acupuncture. They are often irritable because they are in a lot of pain. I used to spend a lot of time explaining what acupuncture is, and how it works, but they really weren’t interested. They just want to know if I am a nice person, if I will listen to them, if I can help them and accept their idiosyncrasies. For example, there are some vets who don’t like the door to the treatment room closed, they don’t like confinement. Some have to be able to see the door at every minute, and some have to have their back against the wall. These are things I understand about them and do my best to accommodate. This goes for any of my patients, not just vets. All my patients are unique and have unique needs.
I also work with couples to help them conceive naturally or support them when they are undergoing fertility procedures. Fertility patients are extremely emotional. The emotional ups and downs of waiting every month is stressful because they want that baby so badly. I understand the emotional toll it takes on them.
And I work with patients who simply want to optimize their health.
MG: What you are describing is so different than standard medicine where appointments are usually 15 minutes. Although some Western doctors try to work holistically within the constraints of the system, I rarely feel “seen” or understood in the ways you are talking about. The view of the patient as a whole that you describe in Chinese medicine is missing.
AB: Well, to be fair, standard medicine is different now than it once was. It used to be you would go see the family doctor, and he or she would ask, “How are your children? How is your job going? Have you read a good book lately?” You might say, “my stomach has been bothering me,” and they might ask, “Well, are you still eating a lot of chocolate and drinking six cups of coffee a day?” And you might say, “Well, yeah.” Then he may say, “Well, you might want to cut that out.” That is what family doctors used to be like. They knew you well because your relationship extended over decades. Most of us no longer expect that kind of personal relationship with our doctor. Our primary doctors come and go. A specialist may have the worst bedside manner, but if he can diagnose what is going on with you, you are okay with that. On the other hand, having a personal relationship is an integral part of my treatment. It develops naturally over time. It’s not optional.
MG: Can you explain the various forms of Chinese medicine?
AB: Chinese medicine includes acupuncture, moxibustion, cupping, heat lamps, gua sha, massage, and herbs. A lot of practitioners today only do acupuncture, which is effective on its own.
MG: But you do everything.
AB: Well, I feel I don’t get the results I want with just acupuncture. Years ago, I started my practice sharing a chiropractor’s office. I loved working with him. He helped me to understand muscles and muscle groups, nerve pathways and the vertebrae, pressure points, and muscle reactions. I rely on the traditional meridians and points but when it comes to pain, I add body work and massage and when inserting needles into points, I often look for a muscle response in addition to an energetic response.
MG: What is acupuncture? How does Chinese medicine work?
AB: Acupuncture uses very fine needles inserted at specific points along meridians, the pathways in the body through which life-energy or qi flows. These are not physical pathways, but energetic pathways that have been a part of Asian medicine for thousands of years. There are many different techniques and schools within the field of acupuncture. For example, there are Chinese, Japanese, and Korean styles, and there are many different methods of choosing points and of needling. My style relies on Traditional Chinese Medicine.
I look at treatment in two ways. First, I address the patient’s immediate concern, and then I address the whole person, including their mental and emotional state. For example, if someone comes in for back pain which is the most common condition I treat, I will treat their back pain, but I may also end up addressing their grief. In the past few years, I have treated people who have had Covid for fatigue, respiratory conditions, and digestive problems, and I often had to address their anxiety as well. Treating the whole person is unique to Chinese medicine.
MG: What is moxibustion?
AB: Moxibustion is the burning of the herb mugwort over an acupuncture point. You stimulate the point with the heat from the burning herb rather than with needles. There is a special way the mugwort is processed so that when you burn it you achieve the cleanest burn. It is also aged. The older the mugwort, the better. There are many different ways to burn mugwort or “moxa” as a treatment. The most common one is using the stick form which is shaped like a cigar. You light one end of it and hold it near the acupuncture point you are wanting to warm.
MG: Tell me about cupping.
AB: Cupping is a procedure for pulling stagnant blood out of muscle tissue. Special glass suction cups are applied to the body so that the blood is forced out of the muscle tissue being treated. It’s almost a lymphatic way of moving blood and fluid.
MG: And what about herbs? Do you create your own herbal formulas?
AB: I don’t do as much of that anymore. Instead, I use a high-quality line of prepared herbal formulas. I used to send my own formula of loose herbs home with patients, but they wouldn’t cook them as directed. It takes time and effort, and they can be strong smelling, so they didn’t use them. I needed something in pill form my patients would actually use and benefit from.
MG: So how do you diagnose a person?
AB: After practicing almost 30 years, I’ve gotten to the point where upon meeting a person I have a good idea what is going on with them. When I diagnose a patient, I consider the eight principles. And I look for disharmony in any of the organs—the kidney, the spleen, the heart, lungs, and so on. The eight principles are heat, cold, yin, yang, internal, external, deficiency, and excess. Also, there are six pathogens that can invade the body: wind, cold, heat, summer heat, damp, and dryness. If someone is cold all the time, I will do warming treatments. I notice if they are deficient or have a form of excess, and I will work to balance their body. The American population in general is damp so I am always looking for that.
MG: So, you assess a patient based on what they tell you and how you observe and experience them?
AB: I base a lot on appearance, skin color and quality, muscle tone, how they move, how they look, their affect. I also learn a lot about imbalances and overall health from touch and from body work.
MG: What are tongue diagnosis and pulse diagnosis in Chinese medicine?
AB: Tongue diagnosis is simply observing the color, shape, and texture of the body and surface of the tongue. It is a way of showing what is going on internally. The pulse is a much more subtle way of diagnosing a patient's condition. The speed, depth, and force all indicate different things. Tongue diagnosis and pulses are much more important for prescribing herbs. With acupuncture, it is not as important. If the patient is having symptoms I can’t quite figure out, then I will look at the tongue. I will do pulses if I need confirmation of my diagnosis.
MG: Do you work with regular MDs or coordinate with them in a patient’s care?
AB: I sometimes work with oncologists and other MDs. Cancer patients are very challenging. They have issues with digestion, pain, fatigue, and nausea. Having cancer is very difficult and patients need emotional support through their whole treatment process. My interest in cancer care was born out of a strong desire to find the best way to help those in these difficult circumstances. If I only worked with cancer patients, it would be a very fulfilling practice for me.
MG: Does your treatment differ according to the type of cancer the patient has?
AB: I can have five breast cancer patients, but each one of them is unique and will require a different treatment approach. Each patient can have the same western diagnosis but will end up with dramatically different treatment plans in the Chinese system. On the other hand, you can have five patients with five different western diagnoses, but they end up having the same Chinese acupuncture or herbal treatment plan. They may all be deficient and struggle with anxiety, for example.
MG: I love that Chinese medicine is so personalized. The patient is treated as a unique individual. Western medicine tends to base treatment on “best practices,” or a one-size-fits-all approach driven by managed care and insurance coverage. I know you treat a lot of people with back pain but what about other kinds of pain?
AB: I treat many kinds of pain—back pain, knee pain, joint pain, and a lot of people come in for headaches.
MG: Are you successful with headaches?
AB: Actually, headaches are not that difficult to treat. A lot of headaches end up being tension headaches stemming from neck and shoulder muscle constriction. When I relieve that constriction, the headaches go away. Then, some headaches are stress related and diet related. I may suggest lifestyle changes for those patients. And, occasionally, some patients I am not able to help.
MG: Tell me what happens during an initial visit?
AB: The first visit is an hour and a half. I usually spend the first half hour going over the patient’s medical condition, their history, and what brought them to me. I will then do acupuncture on one or both sides of the body depending on what feels appropriate. If I do the back, I will often combine a massage with acupuncture. Tui na, or Chinese massage, gives me additional information. I can tell a lot about what is going on with a person through touch. Then we talk about a treatment plan. I may suggest lifestyle changes and I may prescribe herbs.
MG: What do you love about what you do?
AB: It forces me to be fully present. I can’t do what I do without being 100% focused on the patient and the process. I love that feeling and I love helping people.
At the time I first studied acupuncture in the early 90s, it was a kind of fringe occupation. We all went into it for the love of it. We didn’t expect to make much money doing it, much less support ourselves. At the time, there was no recognition in mainstream medicine of the benefits of Chinese medicine, and there was no insurance coverage like there is today. Over the years there has been a growing acceptance and appreciation, among the general population and mainstream medicine, of the beauty, sophistication and effectiveness of acupuncture and Chinese medicine. I am so grateful to have the privilege and joy of helping people improve their health and their lives through this ancient method of health and healing. I have never done anything else and there is nothing else I would rather do.
Anne Biris, RAc practices at Eastern Integrative Services at 2300 Washtenaw, Suite 101 in Ann Arbor and 24534 Hass Street in Dearborn Heights. To make an appointment you can reach her at (734) 761-5402 or visit her online to learn more at easternintegrativeservices.com.


































Community acupuncture, on the other hand, offers a sustainable and fiscally sensible solution to treating as many people as efficiently and effectively as possible. Evan Lebow-Wolf, co-founder of Ann Arbor Community Acupuncture (AACA), told me briefly about the difference between community acupuncture and private acupuncture. When I asked him whether he feels like there is anything missing in the community acupuncture approach that is available in private acupuncture sessions, he replied with a firm and resolute “no.”