By Ashton D. Justice • Photos by Mary Bortmas
“We can’t solve problems by using the same kind of thinking we used when we created them.”
–Albert Einstein
Life is hard and yes, terrible things can and do happen, oftentimes to people who do not deserve it. Denying trauma and trying to inspire people out of its impact, both individually and collectively, has been the go-to method of dealing with trauma for generations.
We live in a world where trauma is commonplace and oftentimes inevitable. And, of course, history is repeated when members of society at large follow suit in paying a bit of lip service to the issue but not really talking about it. We judge those affected by trauma and avoid facing trauma and those impacted by it at a great cost to ourselves and to others. The most significant cost being the lives and well-being of those affected. Could there be another way to help people?
PTSD (Post Traumatic Stress Disorder), which results from acute trauma, and C-PTSD (Complex Post Traumatic Stress Disorder), which results from the presence of chronic, unrelenting traumas like child abuse or neglect, domestic violence, systemic racism, sexism, and homophobia are increasing in prevalence and severity. Trauma is all around us, showing up in “typical” families, and in more obviously scarred families. There is trauma in divorce, illness, dislocation, injuries, childhood cruelties, middle school tribalism, work-related failures, unemployment, the loss of a loved one. The disorders associated with trauma affect all of us, in so many ways.
Enter, or rather re-enter, psychedelics. A non-exhaustive list of commonly known psychedelics include: MDMA, Ketamine, Psilocybin (more commonly known as Magic Mushrooms), Mescaline, LSD, Peyote, DMT, Ayahausca, and even Cannabis. Until 1970, when all psychedelics were classified as Schedule 1 drugs in the Controlled Substances Act, psychedelics had been used, with some success, in treating a myriad of conditions, including PTSD and other trauma-induced disorders. In recent years, there has been a robust resurgence of interest and experimentation surrounding medicinal psychedelic usage, also known by other terms including, but not limited to, plant medicines, transformative medicines, and entheogens. Cutting edge thinkers within the medical and psychiatric communities are leaving the traditional “cures” of pharmaceutical drugs and talk therapy behind in search of safe and effective solutions. In recent years, it appears many researchers and practitioners alike are independently arriving at the same conclusion, that psychedelics and the altered states of consciousness achieved by them, could be a significant and meaningful part of the answer.
Southeast Michigan is a hotspot for these alternative trauma treatments and there Is a small trove of qualified doctors and licensed practitioners pioneering varied means of treatment through the use of psychedelics. These treatments are available in an array of settings including fully supervised in-clinic treatments, multi-day retreat-based treatments, and practitioner-guided outpatient treatments self-administered by patients in their own homes. Practitioners and patients alike are seeing success, and many traditionally trained psychologists and psychiatrists are taking notice. What follows are conversations with three pioneers in the area in the field of psychedelic-based therapies and treatment.
Megan Oxley, M.D., a former emergency room physician at the Detroit Medical Center, left the hospital setting in 2016 to open Michigan Progressive Health (MPH), a ketamine-assisted psychotherapy practice with offices in Royal Oak and Ann Arbor. “What we do at MPH is help patients get to the root cause of their symptoms. It’s not because you have a chemical imbalance in your brain. There’s a lot of things that have come before it in your life and your lifestyle that have led to this place, and we are trying to sort out why it is they are feeling this way so they can be empowered to change it.” In discussing the altered states of consciousness achieved via psychedelics, Dr. Oxley has continuously observed in patients “an opportunity to look at your problems differently or be in a different mindset when looking at your problems.”
While having an appropriate mindset about personal problems is a concept people understand, achieving it when plagued by the impact of trauma on the human brain can be an insurmountable task for many with (C)PTSD. Fortunately, the off-label use of ketamine injections has proven to help many MPH patients achieve this. As Dr. Oxley described it, “Creating new connections in your brain and reviving old ones that have been left in the dust…there’s physical connectivity and a psychological benefit in the brain that allows for seeing things from a different perspective.” Coming up against a lifetime of socialization, understanding and managing the disorder is a journey for these patients, a journey which appears to be facilitated by continued treatment with psychedelic medicines. “The biggest problem in our society is not recognizing trauma for what it is…we are very emotionally restricted and that’s how we teach our children.” When asked what sources of trauma she sees coming through her doors the most, this writer was taken aback by her response: “The most common is just life…and not recognizing trauma for what it is.”
Patients coming through the doors at MPH are desperately searching for a deeper understanding of the trauma and resulting conditions influencing every aspect of their life and hope to find a solution that will provide a way through the darkness and into light. Referencing her deep dives into the profound work of author and physician, Dr. Gabor Maté, Dr. Oxley said, “I believe that most of the conditions are rooted in trauma: ADHD: rooted in trauma. Addiction: rooted in trauma. Autoimmune conditions: rooted in trauma.”
Furthermore, elaborating on the relationship between trauma, mental health disorders, and autoimmune disease, she said, “The condition is just the label created by psychiatry for the sake of convenience and billing. That may be an unpopular opinion, but it’s not that important in the grand scheme of things. Here in the clinic, we have fixed these conditions that have basically been stemming from the root cause.” In talking with Dr. Oxley it became increasingly clear people do not identify their conditions as being a result of trauma. And society supports the pattern by touting bad luck, faulty genes, poor lifestyle choices, and really anything but trauma as the root cause for debilitating conditions. Dr. Oxley believes the western medical establishment has contributed to further this notion as well. “We saw the patterns, but no one talked about it, and nobody was curious.”
Somewhat in its infancy, much remains to be understood about how and for whom these treatments can be most fruitful. As an example, Dr. Oxley explained, “There is some early evidence that people with childhood trauma, which can be emotional or physical, respond better to ketamine than people who don’t, which is really interesting, and is yet to be sorted out by science.” MPH is actively researching this phenomenon now.
Patients seeking treatment at MPH are subjected to a series of assessments and exams to make sure they are eligible to safely receive off-label ketamine treatment. Once a patient has been determined eligible for treatment, a highly individualized treatment plan is developed. Most patients receive approximately six-to-eight in-clinic treatments over the course of several months, with follow up visits in between to track progress. While the use of such powerful medicines would ideally be used in tandem with a long-standing therapeutic relationship, Dr. Oxley acknowledges this is not always possible, and the reasons are quite tragic. “We strongly recommend that patients are working with a therapist, but we do see a lot of people who have been either disenchanted or disenfranchised by the therapy system.” Even without an established therapist, patients and practitioners alike see results that previously felt impossible. “Once you started seeing people get better with ketamine you had to start explaining things that weren’t explainable with western medicine.”
And maybe a healthy degree of separation from western medicine is required to understand and achieve maximal benefit from these medicines. Historically, psychedelic experiences were often deeply sacred and as much part of an emotional and spiritual journey as a medicinal treatment. It seems there was something to the way these medicines were consumed with such intention in more ancient times and Dr. Oxley believes holding close to those traditions should be part of the protocol. “I would like to see these medicines be used with reverence the way they were for thousands of years before we got to the place where we are at…and I think they should definitely be legal.”
With clinical psychedelic treatment legally restricted to the off-label use of ketamine at this time, and out of pocket costs ranging between $5,000-$10,000, decriminalization and legalization of psychedelics could be key to addressing the mental health crisis on a scale from local to global. Dr. Oxley acknowledges this, stating, “That’s the biggest problem with what we do…we don’t see the patients that probably need ketamine the most…Accessibility is my next big hurdle to tackle.”
And tackling it she is. Amid the Covid-19 global crisis, Dr. Oxley began the process of establishing a non-profit organization to make psychedelic medicines legal, available, and affordable to all who need and want to explore them. Regulatory changes concerning legalization and insurance coverage won’t just help patients with affordability and access. Changes such as these would allow licensed practitioners to legally offer a more diverse array of healing psychedelic remedies such as LSD, MDMA, and psilocybin in a clinical setting without risking legal consequences and loss of licensure.
While an expert in her field, Dr. Oxley is also a lifelong student of it, choosing to look at every case as an opportunity to learn. “Every patient teaches me something new about depression, about PTSD, about ketamine, about psychedelics, and about life, and I try to carry that forward to future cases. Always learning.” One of the most important things Dr. Oxley has learned is to include a personal approach to bringing psychedelic medicine into the local conversation about treating trauma and normalizing the use of psychedelics asserting, “There is an onus on those of us in this place to be more open. Like, I’m a better mother because I did mushrooms.”
When asked what the most important takeaway from our conversation should be, she said, “What people need to know is that these medicines are inherently quite safe and extraordinarily helpful, and our society is suffering more and more with mental illness and this is one really big way we can make a difference in not suffering…The root cause is our toxic culture. We work too much, we eat too much, we drink too much, we do everything too much because we are trying to distract ourselves. Human doings not human beings, completely out of touch with our human bodies.”
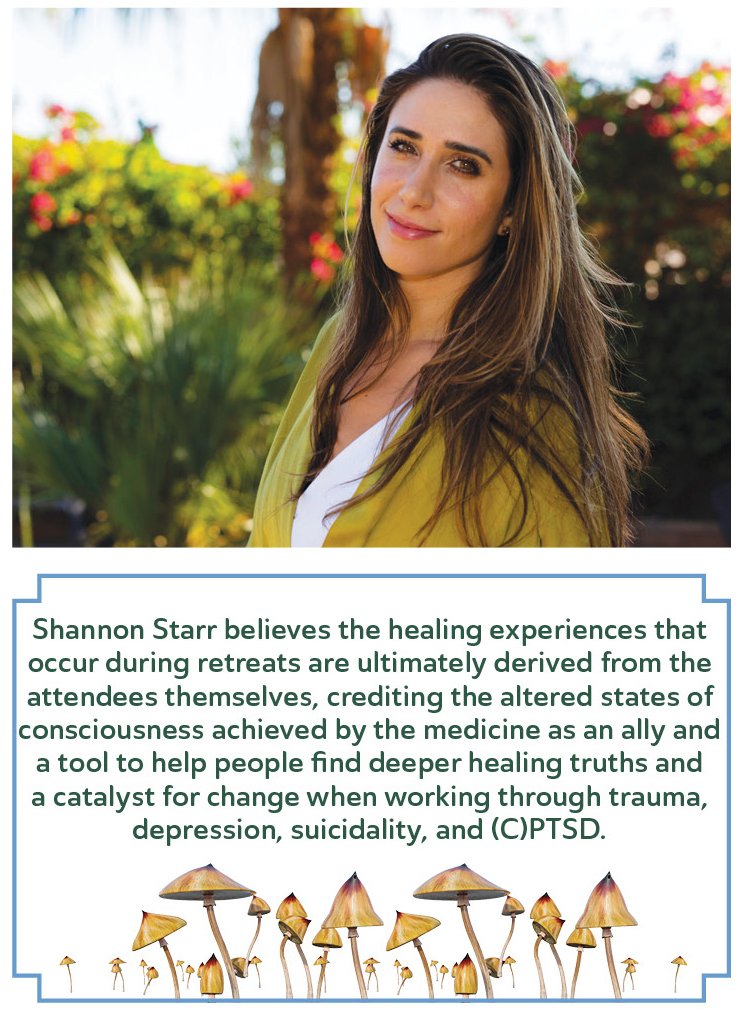
Seeking a consciousness-based and more relaxed clinical approach to psychedelic treatment, Southeast Michigan native and Nurse Practitioner Shannon Starr PMHNP (Psychiatric Mental Health Nurse Practitioner) founded Floresta in 2021 with “a team of clinicians, doctors, coaches, pioneers and those that dare to be the change that is required within mental health and psychiatry.” With offices in both Michigan and Florida, Floresta offers monthly ketamine-assisted psychotherapy retreats across the United States.
Dedicated to doing her part in improving the human condition, Starr was transparent in sharing her position on how psychedelics produce results so vastly different than traditionally accepted means. “Through these medicines one can create change that is not linear and can really allow for a way to regain choice and power and thrive in one’s life and not just survive…energetically treating the whole person.” During these two-to-four day immersive retreats, the Floresta team takes an open and energetic approach to working with anywhere from six to up to twenty attendees, finding that “transformation can occur much more rapidly when we are not trying to control it, limit it, or have any conclusion on what it looks like.”
These retreats include other spiritual and mindfulness-based activities such as yoga, breathwork, guided nature walks, and TCM (Traditional Chinese Medicine) sessions to enhance the overall healing experience and create a “safe and reverent space” for the ketamine treatments. Starr believes the healing experiences that occur during retreats are ultimately derived from the attendees themselves, crediting the altered states of consciousness achieved by the medicine as an ally and a tool to help people find deeper healing truths and a catalyst for change when working through trauma, depression, suicidality, and (C)PTSD.
At the outset of her career, Starr planned to take a functional and nutritional medicine approach to treating psychiatric conditions. That course changed when she began working with psychedelics in 2017. Committed to demonstrating the level of vulnerability she encourages in her patients, Starr shared that her passion for these medicines was born out of a journey to find help and solutions for her own struggles with mental health and related physical conditions. “In my first psychedelic experience I could perceive the capacity for change that could be created in a way that moves so much faster, and I love moving quickly, efficiently, and safely. Working with plant medicine and allowing for more of these mystical experiences, that allows and unblocks different ways of perceiving reality, and a lot of trauma and psychiatric conditions aren’t necessarily linear.”
Keeping in mind the non-linear gradual nature of healing, Floresta hosts regularly scheduled integration circles for patients to attend indefinitely at no cost following the retreat experience. This also allows the Floresta team the opportunity to provide continued support and to observe long-term outcomes. When asked to share some examples of common, powerful outcomes she has seen, Starr ‘s response was immediate. “Working with clients with acute suicidality. I had a client at a retreat saying if this didn’t work, she was going to look into legally euthanizing herself. And having that totally changed, coming in feeling completely suicidal and leaving full of hope and feeling joy. That space of worry and constant rumination is now a space of calm and patience and less reactivity.” Counting herself lucky, you could feel the sincerity in Starr when she said, “I am so happy that I am alive in this lifetime where I get to offer this treatment and really see how it’s healing and helping.”
Describing ketamine as an “algorithm disruptor,” Starr recounts other common outcomes including patients finding love for themselves, developing a routine that fosters healthy living, and an increase in mind-body connectivity. With patients with depressive symptoms, she regularly sees the lack of motivation and fatigue open up, so people can do things to move their lives forward. In (C)PTSD patients the trauma response, reactivity, and hypervigilance transforms into a space of calm and relaxation, allowing the whole nervous system to relax. (C)PTSD patients are able to have a softer response and see reduction in panic attacks, nightmares, and other symptoms that have plagued them and interfered with their life and functionality for years. With psychedelics, they can discover that it is normal for the body to be relaxed and allow relaxation to be their new baseline.
While Floresta only offers ketamine treatments at this time, Starr is excited about the direction things are headed in -- the legalization of other psychedelics, particularly psilocybin. Still, she worries it is not happening fast enough for people suffering now. In order to help these people sooner rather than later, Starr and the Floresta team are currently exploring options for hosting retreats in places where psilocybin is legal, such as Jamaica. Echoing Dr. Oxley’s sentiments, Starr also believes that while some people could find success using psychedelics in a recreational space, others would not. So, this creates a need for safe and sacred settings, as well as proper educational resources made readily available, for individuals choosing to utilize psychedelics as part of their journey to healing and wellness.
A steadfast pioneer in this cause, former Licensed Professional Counselor, Board Certified Music Therapist, and Founder of Blue Sage Health Consulting, Julie Barron, has been instrumental in bringing the magic of plant medicine and psychedelics into the public eye and providing quality training to interested individuals as well as emerging psychedelic practitioners right here in her home state of Michigan. Her first task was to decriminalize plant medicines in Ann Arbor. In 2021, newly elected Washtenaw County Prosecutor Eli Savit made a bold move, essentially decriminalizing possession or small-scale distribution of entheogenic plants and other naturally occurring psychedelics, as well as supporting the expungement of old criminal convictions arising from entheogenic plant offenses. When looking at progress such as this, the contribution of Barron’s 10 years of activism in this arena can’t be lost upon us. While doing away with criminal consequences for using these substances is a huge step forward, there is still a long road ahead in making these medicines and treatments available to all who need it. With emphasis, Barron put it quite simply, “The goal is access. For all who want it with the focus on the most vulnerable people among us first.”
A lover of plant medicine since she was young, Barron began training to work with transformative plant medicines and non-ordinary states of consciousness during her graduate studies, crediting this work as defining her path as an out-of-the-box thinker. Upon completing her formal education, Barron knew healing does not occur in a vacuum and felt she could not do this work without “working on the community base” to decriminalize and legalize access to these medicines, particularly psilocybin.
Barron considers psilocybin the “whole package,” holistic on every level in working with individuals plagued by (C)PTSD and trauma. She envisions a treatment landscape that incorporates a therapeutic process around plant medicine work, including supervised macrodoses (larger doses with more profound psychedelic effects) of psilocybin followed by self-administered microdoses under the guidance of a practitioner.
Looking back on decades of work in this field, Barron cites neglect and emotional, physical, and sexual trauma as the primary precursors to (C)PTSD that she sees. Additionally, she finds the more complex the trauma, the more complex the case, necessitating a team-based, long-term healing approach. To meet this need, Barron works as a consultant to the therapist and client. “It’s hard to figure it out on your own and there needs to be people helping them figure it out.” Multiple times per year Barron offers formal training seminars to therapists, teaching them how to help their clients on their journey to help themselves with these medicines.
In discussing outcomes, Barron reflects upon her nearly three decades of work, summarizing it with a powerful statement that includes both the patient and the therapist: “The greatest gift that comes out of psychedelics…is the interconnection between mind, body, spirit. Overall, the people I work with do shift, and as a therapist that is my guide to success.”
With high costs and lack of insurance coverage creating a massive socioeconomic disparity in formal clinical access to these life changing and often lifesaving treatments, people have become desperate and begun to pursue them on their own. Brett Johnson LMSW (Licensed Master Social Worker), a trauma informed therapist at Peaceful Mind Counseling in Dexter, has worked with clients who have had to take this path to help themselves achieve a pre-trauma level of functioning. Johnson approaches these clients in an open and supportive way. “As mental health professionals, it’s important we recognize existing barriers to treatment, and we can take an open approach in supporting clients who seek this type of treatment on their own and notice a benefit. People have reported positive change attributed to the use of psychedelic medicine, and continued research and progressive policies may help to eliminate treatment barriers, expand the types of services provided by mental health professionals, and ultimately, improve the lives of those who find this treatment beneficial.”
Trauma is not new, but therapists are applying new ways of thinking to the problem. Body/mind modalities and somatic-based therapies have moved the ball forward in treating trauma. It began with Wilhelm Reich in the 1950’s, moved on to Alexander Lowen’s Bioenergetic Therapy in the 1960’s, Arthur Janov’s Primal Therapy, and Ida Rolf’s Rolfing, in the 1970’s, and then the somatic experiencing therapies, EMDR, and sensorimotor therapies in this century. Cutting edge therapists over the last 70 years have worked hard to understand the roots of trauma and neurosis. Now, finally, psychedelics have become an accepted part of the toolbox for impacting the treatment of trauma. There is a sense that psychedelics are a potential game changer in working with trauma, provided that one is working with conscientious and responsible practitioners. We can all be grateful to the practitioners who are charting these new paths with psychedelic treatments, and we can also be grateful for these plant-based medicines, themselves.





































Peace is the felt experience of an inner sanctuary—a place of tranquillity and calm detachment that you can always access. Equanimity is composure under stress. It is a deep internal knowing that no matter what happens you will handle it and be okay.