by Angela Maderas
Editor’s note: Angela Madaras shares the story of her near-death experience(s), and offers compelling testimony about the effectiveness of hospice care and complementary approaches for her healing and ongoing health. Interviews with two practitioners provide rich background about the philosophy, training, use, and outcomes of these approaches. The title refers to a phrase that Angela kept repeating while “out of mind and body.” She explains, “My husband and the team caring for me used it as a motto, and eventually he created wooded plaques for eight caregivers that said ‘Be Brilliant.’”
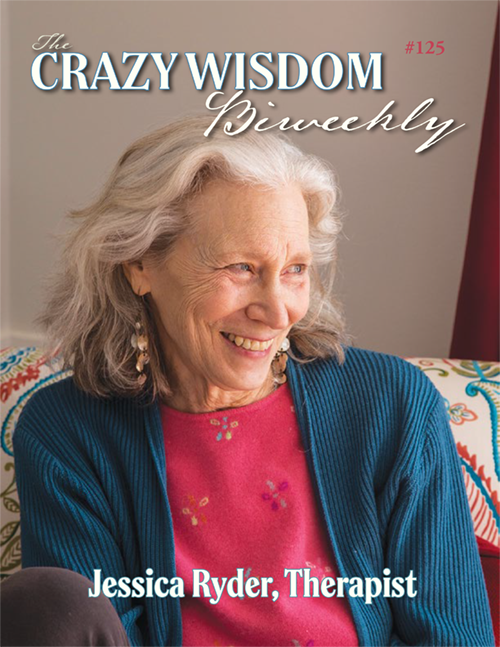
The word “hospice” is one of those terms to which each individual has a unique and palpable reaction. For some it brings a sense of fear or uneasiness. In others it arouses tender memories of a past experience as it relates to a family member. For a lucky handful, their faces light up when engaged in a conversation regarding end of life care in the capable and compassionate hands of hospice staff. These blessed few seem filled with peace and joy in the face of this word. As with all of life, we perceive it through our own lenses, which shape how we feel about any given situation. My personal experience and perception of hospice is filtered through many different experiences with friends, family, and from volunteering for a children’s grief program I helped create with Hospice of Asheville, North Carolina, in the early eighties. I’ve had several close friends cared for by their loving hands during end stages of life, and three of my grandparents and my mother-in-law were in hospice care before they passed out of this earthly plane with loved ones by their side. I know what it takes to be a volunteer and how impactful it was to receive comfort and care, both in facilities and in-home. I was impressed with each instance. I developed an incredible amount of respect for the doctors, nurses, volunteers, and all those who provided ancillary and complementary services, including animal companionship, social work, music therapy, massage, and housekeeping. There are several local hospice options, but my perspective in this article is based on my experience with Arbor Hospice, which offers high quality services and has an intense training program for paid staff, professionals, and volunteers alike. If you are interested in being involved with one of seven local hospice organizations, you can find them on the internet. I worked with Arbor Hospice because I had experience with them when my grandmother passed, and they are located closest to my home.
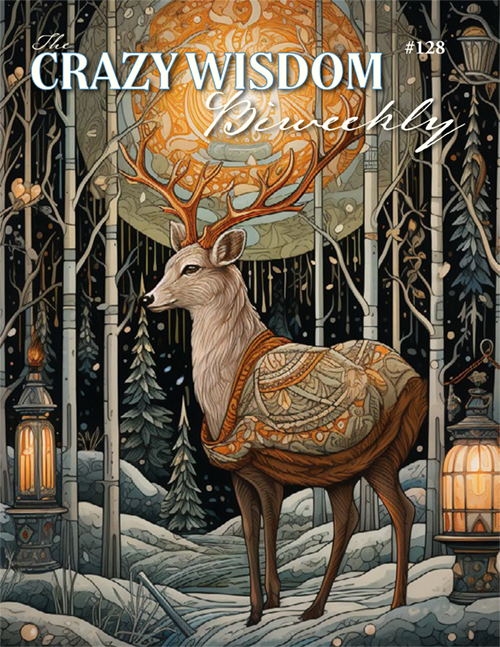
After early- to mid-adult life took me through its many twists and turns, I found myself desiring to be more involved with hospice as a volunteer, and/or in designing a respite hospice farm from a patient’s perspective. I envisioned a space (a home) where not only patients, but family and caregivers, could have a place to go when they needed a break from their normal routine. One set in a peaceful, farm-like setting with private rooms, family cabins, communal areas, and an abundance of natural areas, gardens, and walking paths. This vision came to me during two years of studying end of life care from a spiritual perspective, while preparing to be of service as a lay monk in the Zen Buddhist tradition. The sangha (community/temple) where I studied was deeply engaged in helping the dying transition, as well as organizing post-death ceremonies. Sadly, my own health challenges kept me from serving in this way; instead, I went back to school in my late forties. I wrote a paper on hospice for a sociology class while I continued to read and learn as much as possible about death, dying, end of life care, palliative medicine, burial planning, and my own mortality. Around this time I literally breathed in my Grandma Vera’s last breath out. In a typical hospital setting this would not have been possible, as she would have been hooked up to all kinds of cumbersome tubes and breathing apparatus. My experience with her was transformative, in that it embodied sacred rites of passage from one realm to the next. This touched me in most profound ways. While in school I continued to be challenged with a life-threatening disease with its own set of circumstances, which affected every major organ system in my body to the point I was unable to work, or live “a normal life.” I was facing the end stages of my time on earth…or so I thought.
One day in late June, 2017, I awoke in the hospital after a year of medical issues that affected even the simplest of tasks: reading, communication, walking, balancing my checkbook, remembering to take medication, cooking safely, keeping up with housework, socializing, sleeping, eating, driving short distances, and gardening. I was told I had lived through a couple weeks of some pretty horrible grand mal seizures (five we know of, and a plethora of mini seizures over a year or more that went undetected) and a whole host of other issues that had me sent from one hospital ICU to another. That hot summer day, I found myself preparing to go home under Arbor Hospice’s care, unsure of how long I would live. I do not remember most of June or July but I do remember approaching death and seeing incredible lights – an indescribable prism of colors that kept me on the edge of this world and the one beyond. In short, I came to death and danced with it in the light of this brilliant world and beyond the universe as we know it. I came back and survived for some unknown reason, but was still “tripping the light fantastic” between both realities, and doing it on my own terms. Hospice provided me the support needed to do this, over a six-month period, in the comfort of my own home. The entire hospice team has been a saving grace for me and my family. They gave me the hope and freedom to mend.
My nurse, doctor, social worker, and the volunteers and massage therapist(s) allowed me to find comfort in a safe and familiar space with loved ones. Because of this type of self-directed care, I was able to control the medications I did or did not take, the treatments or medical interventions I chose, how I wanted to treat pain and discomfort, how to attain quality sleep, what and when I wanted to eat, and so on. All these things are impossible in a “normal” hospital setting. The use of complementary approaches, such as therapeutic massage, assisted in the healing process, as well.
Hospice is not just about supporting those who are six months from death. In fact, around thirty percent of patients do not die during their first time in hospice. Hospice provides palliative care and hope, with the goal of helping the patient LIVE life with the highest quality possible, in their given circumstances. There are many interesting studies and statistics on the Arbor Hospice web site, at www.arborhospice.org. An excellent book to read on this subject is one every person, regardless of age, should read, especially those in the medical field: “Being Mortal,” by Atul Gawande. There are many others on the subject, but I find this one easy for anyone to read, and most relevant to our time and generation.
For me, natural medicine has been my preference, as time and funds allowed. The act of being nurtured in a therapeutic way, with human hands, is healing for all individuals, but especially for those with a dwindling flame. Natural modalities of body work are helpful for people suffering from pain and illness, whether one prefers acupuncture, massage, craniosacral therapy, reflexology, polarity therapy or other energy work, or chiropractic adjustments. At this time, hospice settings are limited in what they are able to provide, based on what resources they have to work with and the insurance guidelines of a particular state. Medicare, Medicaid, and many secondary insurance companies pay for most of hospice care, up to a certain point. Fundraising efforts and grants also fund some facilities, including Arbor Hospice. There is a growing concern that the funds for these types of complementary services will dwindle as our aging population increases. This will affect everyone, regardless of age or social standing. For example, imagine being an eight-year-old child with terminal cancer, and in horrible pain. Now imagine receiving a massage for that pain, which helps lower pain medications and allows for a better sleep. I want this for all those who suffer.
Hospice is a lifeline and a safe space that allows for room and time to heal and/or die in peace. Providers focus their energy and resources on assisting the patient in the healing process, so death can be postponed. But if death is meant to be within a six-month period of time, they will help with that process in a non-judgmental, positive, compassionate, supporting way that does not currently exist in most modern Western medical culture. I find great comfort in this, as do my loved ones.
I especially want to focus on what hospice can provide in the area of massage therapy, because this has been a most helpful tool in so many ways, including for easing pain, helping with sleep, promoting bowel movements, relieving stress, and decreasing anxiety. Massage and natural modalities have been around for thousands of years. Our Western culture is just now acknowledging the facts and data proving how helpful and healing these treatments can be. I know that I respond to massage and energy work quite well, and prefer this over medications like morphine. However, I want to know I can take morphine if the natural modalities are not effective enough. The two combined offer me a plethora of benefits, as mentioned above. I often say that, “It is a good day when I can eat well, poop well, and sleep well, while being relieved of pain in the comfort of my own home and surrounded by loved ones.” Massage, when given by an experienced therapist in the area of palliative care, can be good for the body and mind. My Hospice therapist, Michelle, explained how patients tend to calm down, relax , and find inner peace after a massage. I found this to be true about fifteen minutes after my session began. It was almost instant relief and total relaxation of body, mind, and spirit. Her calm and soothing personality helped as she explained what she planned to focus on during my session. Then she would be silent, with gentle music playing in the background, to allow me to completely relax or even sleep. After a session with Michelle, I would slide into bed and sleep deeply for a while only to awaken fully rested and refreshed.
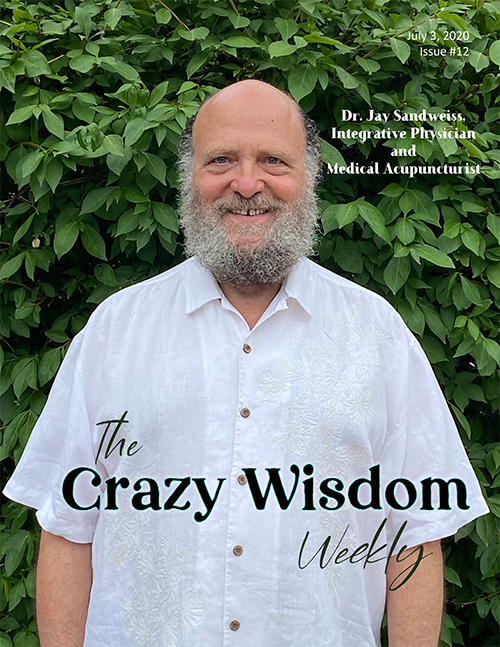
I give my hospice massage therapist, Michelle Chaves-Torres, BC, LMT, much of the credit for overall physical pain relief and general comfort care. I also attribute deep levels of emotional and energetic healing to another professional body worker, Renee Rutz, RCsT, LMT, who is in private practice. I have been working in the area of overall general health maintenance and chronic pain-illness symptom control for around twenty five years with Renee’s assistance and healing hands. Both of these women have helped me navigate this “new world” of palliative care, and helped me to remain fully engaged and thriving while doing so. I have laughed at death and won for now. I owe gratitude for all the many people who have assisted. There is not enough room to write in this article about each individual who has touched or helped me in some way over the past months, but I would like to at least introduce you to both Michelle and Renee, for one of them was with me every week massaging, alleviating pain, and treating secondary issues such as constipation, anxiety, elusive sleep, and so on. I am also occasionally treated by generous family members to acupuncture and other modalities. Rosanne Emanuele (acupuncturist) and Kathleen Dvorak, DC (chiropractor) have also both visited me in my home during this crisis. For this I am extremely grateful. In the following two interviews, you will meet hospice therapist Michelle Chaves-Torres, and massage-craniosacral therapist Renee Rutz.
Michelle Chaves-Torres
My interviews with Michelle Chaves-Torres began in my living room, where we had a massage table permanently set up as a peice of furniture, next to an array of comfy chairs and two overstuffed white couches. Candles were lit, and incense wafted through the house while Gregorian Chants played in the background, offering a peak into what monastic life is like. We softly began our conversation(s) in this way. Follow-up interviews continued over emails and more massage appointments. In this way, you are reading her actual words and not my version of what she said.
Angela Madaras: What and/or who inspired you to work with hospice patients?
Michelle Chaves-Torres: My youngest sister and mom both inspired me to work for hospice. My sister wrote an essay about hospice and gave me a copy to read. She mentioned that she thought I would be good at hospice massage. My mom agreed. I have always been a nurturing individual, from a young age.
Angela Madaras: When did you first begin massage practice?
Michelle Chaves-Torres: I first began massage practice when I attended massage school, in February, 2006. We started hands-on techniques right from the start, and I have been massaging ever since! I started working for a chiropractor out of Belleville as soon as I graduated from school in 2007 – they hired me before I even graduated.
Angela Madaras: Is it more profound working on a person who is in the active stages of dying?
Michelle Chaves-Torres: Yes, it is more profound for me to work on a person who is in the active stages of dying. This is a very special time for the patient and their family. Knowing the family requests for me to be a part of this time makes me feel incredibly honored to participate for both patient and family. It is a gift to work on a person during the active stages of dying. It is very challenging for the body to let go of the spirit during the active phase, and massage is extremely helpful in encouraging relaxation and letting go. To feel and observe this occurring during the active stages is such a beautiful action to be a part of and to witness.
AM: Do you find it challenging keeping your own emotions at bay? What tools do you use for keeping yourself centered and focused?
MC-T: It can be challenging keeping my own emotions at bay. I learned some tools in massage school that really benefit me today in my line of work with hospice. When I am with a patient/client, I “check myself at the door.” That means when I enter into a person’s space to provide treatment for them, I leave myself and my issues, stresses, and ego outside of the home. This allows me to be present in the moment and focus solely on the person and their needs, in order to help them to the best of my abilities.
To stay centered and focused, I try to begin my days as stress-free as possible. This can be challenging, given the fact that driving from patient to patient can be stressful. I listen to peaceful or re-energizing music, drink relaxing tea, and try to think about each person I am headed to visit or just visited with. I reflect on how I can best be a benefit to each person during his or her journey. That keeps me pretty focused throughout the day. I also ground myself each evening when I return for the day. I spend plenty of time out in nature and spend time with my animals. I try to laugh a lot and find joy in every moment. If there is anything I have learned as a result from working in this environment, is to savor every moment for what it is worth, and try to find something beautiful in everything. Many of my patients remind me to enjoy every experience as much as I can, because you never know what may come the next day.
AM: Are patients generally open to being touched? Do they share what they feel openly?
MC-T: Most times, yes, patients are very open to being touched. I have found that many people share how and what they feel openly. Sometimes this will occur for the very first time we meet, but sometimes it can take a few sessions. It just depends on the person. I have had family members comment on things they hear their loved ones say, as if they are hearing these feeling for the first time. This is very healing for the patients during the dying process.
AM: Do you work with family members and care givers?
MC-T: Yes, sometimes families are afraid to touch the patient, because they do not know how. I often will teach family members and caregivers some techniques to provide their loved ones comfort in between my visits, which is beneficial to all. I am sharing the gift of touch with the family, and they learn that they, too, can provide comfort to their loved ones without hurting them. My favorite is showing the little ones, grandchildren, how they can participate with this process, as well, and massage grandma’s or grandpa’s feet. This always brings joy for the patient, the children, and the entire family to observe in action. That makes me happy.
AM: How many patients do you see daily, and what is your area of service?
MC-T: I see approximately three to four patients per day, traveling throughout all areas of southeast Michigan, Monday through Friday.
AM: Please give some me numbers and statistics that readers can identify with.
MC-T: As previously mentioned, I visit approximately three to four patients per day. I try to travel within the same vicinity, to conserve gas and mileage on my car, but some days this just does not work, due to a transitioning patient or other event that may call for my attention. Some days I travel upwards of 100+ miles throughout the week. I work roughly nine plus hours per day as a full-time employee. Our part-time employee visits about two to three patients per day, four days per week, and follows the same travel idea by staying in the same vicinity to conserve gas and mileage, as much as possible.
AM: Do you have one memorable patient or story you can share that is uplifting, or that touched you in a profound way?
MC-T: I have several! I can say working with our pediatric population always does something for me. To see how the massage treatments positively affect a child’s status, to observe and hear their parents’ sense of relief after their son or daughter receives a massage…this actually brings the parents relief in a way that you cannot put into words. That makes me feel good to know I am helping so many people with the gifts I have to share.
I think the reason I have so many memorable experiences with my patients is that there is an exchange that occurs between the patient and me. When I say exchange, I mean I am providing the patient with a listening ear – someone that is unbiased, willing to listen so they feel compelled to share. I learned some interesting things that I never thought I would need to know in my life! However, unbelievably, I remember certain things patients have told me or a certain song that was their favorite one, a certain smell or a food someone described, their memories – that uplifts me; knowing that, even though I helped these individuals into a different realm, there are parts of them that remain here with us. This never fails to bring a smile to my face each time these memories occur.
AM: Can you say that you have experienced actual healing of the body and or disease, to the point of prolonging a person’s life? What does that mean to you?
MC-T: Yes definitely. I know that massage has a profound effect on additional pain management and improves circulation and quality of life, to name a few. I have had several patients that received massage discharge from hospice care into palliative care. I feel good to know I am helping the patients in some way, as well as their families.
It means a lot to me, knowing I am able to improve someone’s quality of life with providing a massage. Families often report that a patient’s days can transform into “really good days” when they know they are getting a massage. That makes me happy, to know I can bring such happiness into a home and share with people in that way.
AM: What would you like the public to know about the program and important services hospice provides?
MC-T: I think it is important for the public to know that the gift of touch is imperative at any stage of life, but especially when in hospice. I feel massage is a wonderful gift to offer to hospice patients because of the enhanced quality of life. It is “forward thinking” to have massage included as part of the plan of careå With the rising popularity to the benefits of massage therapy for many, it is important to know that hospice programs take this into consideration, because it provides many benefits to both patient and family at end of life. Many people do not even consider having a massage at end of life, and I do my best to educate everyone on the importance of massage for the transitioning body, mind, and soul.
Renee Rutz
My interviews with Renee Rutz began many years ago, first with me as a client of Renee’s, and over time, also as a friend. We continue to dialog and discuss the ramifications of complementary and natural therapies versus, and in addition to, allopathic medicine. For this article, I sat with her on my back porch while we ate lunch. It was a gloriously sunny and breezy day at the peak of autumn, when the bronze-tinged maple leaves were just beginning to fall gracefully to the ground. It was the perfect backdrop to the start of our interview. We, too, went back and forth through email with questions and responses. This allowed Renee to refine her answers and offer a very detailed approach to explain how important she feels these complementary therapies are.
Angela Madaras: When doing a craniosacral or polarity treatment, can you physically feel energy moving through a person’s spine and body as you work on them? Can you describe what this feels like?
Renee Rutz: In general, I don’t only use my hands to feel, but rather my entire body and its ability to sense and observe a variety of sensations, energy, tissue qualities, and movements. There can be vibrations of various frequencies. Sometimes I feel a temperature, like warm or cool. There are also densities I can palpate, like hard, thick, or soft. There can be the experience of textures, like stringy, rough, or smooth. There are also patterns of movement that repeat themselves from one part of the body to another. Some of these patterns are ones that I have learned in my professional trainings, and I recognize them as energy in the body that performs a certain physiological function, like craniosacral fluid flow. Some movements are random, and are more related to how an individual is shaped, and what their unique patterns of adaptation and movement are. For example, a person’s gait is an expression of their patterns of adaptation.
Angela Madaras: What are the benefits of receiving body work for those who face chronic and debilitating health issues?
Renee Rutz: It is a way for the patient-client to reside in their body and be more present. Chronic pain and fear can often lead to disassociation. Bodywork helps them feel held, and to know that they are not alone. It helps them to connect with something that feels good. It cultivates a sense of hope, and how they might fully live with their condition, instead of fighting against it.
Bodywork, or any alternative modality, really, offers the patient therapy that is outside the standard medical health theory. In the medical model, the therapy involves going to an expert who figures out what is wrong, makes a diagnosis, and employs a protocol of treatment designed to remove the symptoms. With alternative methods, a different model of health is in play. Polarity therapy, for example, is based on the ancient medical model from India called Ayurveda. Acupuncture and shiatsu are based on the ancient Chinese medical model. Both of these systems see the body as a flow of energies, and the therapy is designed to balance this innate energy. Symptoms are seen as imbalanced energy, instead of obstacles that need to be removed.
This shift of perspective can be quite empowering. The patient can see their condition as something that needs to be rebalanced, instead of a condition set in stone in their being. The patient plays a more active role, and the practitioner partners with the client. Alternative therapy tends to believe that health/wellness is within each of us, and it is a practitioner’s task to help that health and wellness express itself more fully.
Bodywork also offers non-drug pain management, without the adverse side effects of pharmaceuticals.
Angela Madaras: Explain to our readers how trauma release from past events can allow healing on a physical level in the “here and now.”
Renee Rutz: Our bodies are literally shaped by our experiences, and the energy of them can remain stored in the body. How does this happen? In learning anything new we experiment, and these experiments allow us to adjust and adapt until we become competent at what we are trying to learn. For example, when learning to ride a bike, gravity gives us feedback about our balance, and our bodies adapt to it. Over a number of repetitions where we wobble and maybe even fall off the bike, we adapt and learn how to balance and maneuver the bicycle. Eventually, riding becomes natural, and hardwired into our muscular memory. We do it without any conscious control. Some of these same phenomena are at play when we experience something overwhelming or traumatic.
During a traumatic event, the body contracts in a variety of ways to protect itself. Via a series of neurological and hormonal synapses, the brain “records,” or remembers, the experience and what it did to successfully protect itself. The body “hardwires” the successful protective actions. If another experience comes along and feels threatening in a similar way, the body is already conditioned to respond reflexively in the same way that was previously successful, without any conscious control.
These contractive automatic adaptive responses work well for a while. But as a person moves into different developmental stages, these automatic responses may not work as well…or the person is evolving, or new circumstances present, and these adaptive responsive may not be healthy or effective. There becomes a need and desire to change these responses. This requires conscious effort, and often assistance from others, like a therapist, body worker, or a trusted friend.
Body workers are trained to see and feel adaptive patterns and differentiate them from patterns that are innate, functional, and healthy. Adaptive patterns are in the posture, movement, and bio-energy flows in the body. They can be witnessed by tracking sensations and utilizing mindfulness-like techniques. Bodywork uses touch and a variety of manual therapies to bring awareness to what is being held, and to encourage the body to let go. Touch can bring the pattern or shape into relationship to our innate healing potential within. In being in present time with our patterns that our past has shaped, we can let go of the effort and energy that goes into maintaining the patterns and explore what other options we have to behave differently. It is in this process where the energy of the embedded past experience that created the pattern can shift in present time. The client often feels a sense of completion or letting go of the past. The physical shape and movement pattern can be observed as different.
AM: Have you experienced any physical challenges or pain that allows you to be more empathetic while working with a client/patient?
RR: I have several family members who have had lifelong chronic illness. Since childhood, I witnessed their challenges. I believe it is these early experiences that inspired my entire career. I could see that the medical community, as it was when I was a child, could not fully help my family feel completely well. I sensed the anger, frustration and sadness this causes. I could see the disempowerment and hopelessness that arose for everyone when the “experts” could not address or help the issues at hand.
In my discovery of alternative approaches as a young adult, I was invited to explore another way – one that I personally have found to be empowering, gentle, and nurtures people to live full lives in the face of painful chronic conditions.
AM: Do you receive regular body work yourself? What modality is most useful for you as a practitioner as a means of staying open, balanced and energetic?
RR: Receiving regular bodywork is an important part of my health practice. I find that craniosacral therapy greatly supports me as a practitioner. It helps me to connect with that inherent health within me and my wholeness. It gets to the heart of my patterning and gently encourages release. It helps me to feel into my humanity and appreciate this human journey.
AM: How often should a reasonably healthy person receive treatments to maintain good health, and how often do you recommend a person with severe health challenges see a practitioner? What tools do you offer clients/patients as home “remedies” between treatments?
RR: Frequency of visits is an individual choice. How often someone comes in is based on what their goals are, and the ability to put their resources in support of those goals. In general, I find that monthly visits are a good maintenance plan. If you are wishing to change habits or would like to use the work for chronic pain management, then regular visits are probably most effective. One needs to experiment and see what works.
I do suggest activities to try at home. The activities are often created from the content of a session, and are designed to support and deepen the work done in the session. It could be a stretch, a mindfulness practice, or a change in diet. The body is very creative in the ways it can regulate itself!
AM: How does working on a person who has a life threatening illness vary from one who just needs their muscles massaged?
RR: In some ways, it doesn’t differ at all. Obviously, a person with a life-threatening illness brings a different set of concerns to the table than a person with just sore muscles. Both, however, are seeking balance and a greater sense of wholeness. My goal is to be fully present, grounded, heart-centered, neutral, and to hear with as much clarity as possible what concerns my client expresses. From that point the intention of the session is established, and I trust the wisdom of the body to unveil the treatment. How I engage with the client becomes clearer as the session progresses, while I receive feedback from the body via palpation, and from the client verbally.
AM: What advice can you offer those who wish to pursue a career or volunteer in the area of “massage and other natural modalities”?
RR: Receive work from a variety of practitioners and explore a variety of modalities. I find that the work you like to receive is also the work you will probably be skillful at giving, plus it will be more fun.
Study and be continuously curious about the body, its anatomy, its energy and physiology. I believe the language of the body is in its anatomy. If you know the anatomy, and I mean not just in your head, but that your hands know the anatomy, you will be a more skillful practitioner.
Do your personal work. Knowing yourself, your habits and reactions, and how you connect with something greater than yourself, is essential to helping others.
Approach a career in bodywork or other natural modalities with heart and a sense of service. To do it any other way will just lead to burnout.
Learn skills of relating to the body and its energy. Do not rely entirely on treatment protocols. This leads to burnout, too.
Be in the wonder of the body/mind and its ability to heal itself and find wholeness!
AM: You used to be a partner in a group practice. Why did you decide to branch out on your own? How has this changed the way in which you engage with clients? Tell me anything you want our readers to know about your new location and practice.
RR: For 27 years, I enjoyed creating a holistic health clinic and collaborating with other practitioners and support staff. I simply reached a point in my life where I wanted and needed to simplify. I needed an opportunity to explore my work and skills in an environment where I did not need to accommodate in any way. My work needed an outlet where I could just flow with what inspired me, and not have the needs of others influence what I did or how I did it.
I yearned to have more quiet in my work space, which this move has afforded. My focus is more on my clients, as I do not have any administrative responsibilities beyond my own schedule. Having quieter space has supported a deepening of my work. I feel my connection with my clients is more personal and intimate.
My office is in Dixboro Village, which I have discovered to be a sweet and quiet little corner of Ann Arbor! As soon as I arrive in the Village, I can feel myself slowing down.
Author’s Take-Away:
From my own experience, and after interviewing both Renee and Michelle, I believe that therapeutic massage, craniosacral therapy, polarity therapy, and acupuncture can release areas of energy blocks, and perhaps cellular memories of past traumas. I see these techniques as ways to gently clear energy blocks and emotions that keep me stuck in a past moment of time when I was hurt and feeling incredible pain, both physically and emotionally. In this way I am able to be in the present moment, where healing is possible. It is my strong belief that natural healing modalities should be a part of hospice and palliative care, because they alleviate so much of the discomfort while allowing the body either to heal, or to transition with the least amount of pain. I also feel that natural modalities should be fully covered as health maintenance and preventive care for all individuals, and especially as treatment for chronic illness. May this article spark conversations around your dinner table about end of life desires and wishes, and how you want to manage your long term care if facing a life-threatening and debilitating illness. Lastly, I hope each individual sees their inherent ability to heal one’s self while gaining a deeper understanding that life is a precious gem which needs to be polished and treasured. Shine brightly and be brilliant, so others learn they too can do the same.
Related Content:































I grew up in the Midwest. The Midwest isn’t anywhere, it’s a place people come from. If they can. Land-locked, we pretend lakes are great seas and rivers will take us somewhere if only we would go.