By Kirsten Mowrey | Photography by Susan Ayer
In 2013, Professor Ana Baylin found herself in a professional crisis. After training as an M.D. in Spain, getting her Ph.D. in Nutrition and Epidemiology, and working at the U-M School of Public Health, she found herself wanting to do… something else. A colleague encouraged her to enroll in the Faculty Scholar Program (FSP), a year-long educational group. The faculty in the program study recent research on integrative medicine, such as meditation, yoga, and chiropractic, as applied to cardiovascular disease, cancer, chronic pain, and mental health. By exposing professionals to the benefits of other disciplines outside their own, and building bridges based on science between medicine (disease treatment) and health (vitality and well-being), faculty find themselves creating new methods and solutions to patient problems. The program has been innovative and successful, and a key element in the slow but steady growth in the acceptance of integrative medicine at the University of Michigan.
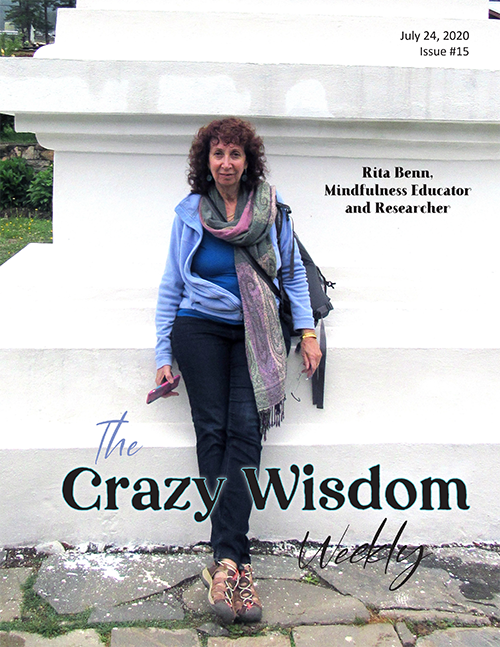
“After 15 years, 150 scholars, numerous programs designed and implemented and countless classes, Rita Benn has persuaded and inspired many of her colleagues of the value of integrative health for all, especially for those who teach.”
Baylin, for example, met Max Shtein, an engineering professor. Shtein was working on designing UV lamps to affect appetite and obesity. As Baylin looked at the implications of Shtein’s lamps, she found herself getting excited. From a public health perspective, the lamps offered an intervention to change local metabolism, affect appetite, and decrease risk of obesity, particularly for healthy people who worked night shifts, irregular hours, and in a cubicle. During the year-long program, Baylin and Shtein began collaborating on an experiment involving the lamps, with Shtein providing the technical side and Baylin providing the public health aspect. They have applied for grants to do experiments, collect data, and research if this could be an effective intervention for obesity. Baylin said “[This was] the best thing. I was in the middle of a professional crisis. [Then] I met Max, and now I’m in a project I love. It opened me to a different way of thinking.”
This class not only resolved Baylin’s professional difficulties, it led her to new innovations that may address a current public health challenge, as well as offer new technologies for health. All that from the work of two scholars in one year. And the FSP has been running for 15 years. What other amazing doors have been opened, interventions and innovations created? What else is possible? And it’s also possible that this very worthwhile program might slowly disappear, underfunded, dismissed, and lost in the University’s Medical School.
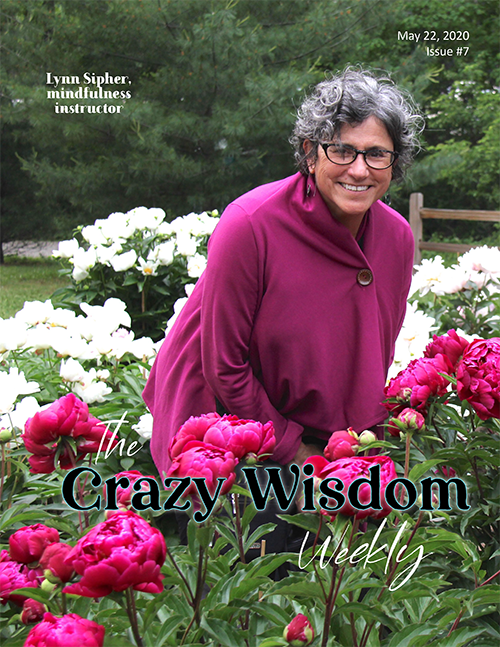
The Faculty Scholar Program is the creation of Rita Benn, Ph.D., and Dr. Sara Warber M.D., with others collaborating. Benn is a curly haired, bright eyed woman, who cocks her head to the side as she listens to your questions. Her home office is stuffed with books, and stacks of paper and journals sit on her desk with a computer and recessed keyboard. It was late summer when we talked, and she, as program director and teacher, was preparing for a new year of scholars and projects.
Originally from Montreal, Benn arrived in Ann Arbor in 1975 to do a Ph.D. in Clinical Psychology and Education with clinical child and school specialization. Upon receiving her doctorate, she traveled to India and worked at Boysville in Clinton before starting her family in 1982. When her first son was over a year old, Benn began work at the Merrill Palmer Skillman Institute for child and family development at Wayne State. She worked with attachment in infants and mental health, developed policies for assessing children at risk for developmental delay and disability, and wrote grants with the state for social services. Her Ph.D. had prepared her well for bringing together the many disciplines necessary to help one- to five-year-old Michiganders to thrive: social work, education, and public health joined in campus collaborations.
“There are usually anywhere from 10 to 15 scholars a year coming from all over the University. Rita Benn points to that as one of the accomplishments of the program. “Faculty have an opportunity across campuses and disciplines to learn from each other. Ours is very broad: art, music, business, engineering.””
In 1997, after years of commuting to Detroit from Ann Arbor, her husband commuting to Jackson, and her three children in elementary school, Benn decided that someone needed to be local, and she left Wayne State. She had heard about a new grant to research Complementary and Alternative Medicine therapies (now called integrative medicine) in cardiovascular disease, given to Dr. Sara Warber, Suzie Zick, and Alana Gillespie at the U-M Medical School. She was invited by her friend Coco Newton (who was featured in the cover story of issue #60 of the Crazy Wisdom Journal, available on its online archive) to a lecture Newton was giving at Parke-Davis, which Dr. Warber also attended and where they were introduced. After meeting Benn, Warber said, “We’ve got to figure out a way to get you part of us.” Benn wrote her job description for Warber and was hired in 1999 to do education-related research for the grant.
In 2001, Benn and Warber wrote a second grant to the National Institutes of Health. Its goal: to bring integrative medicine to the medical school and its allied schools of health. Alternative health use had been increasing among the public since the 70’s but ballooned in the late 1990s. Many patients were using massage, herbs, chiropractic, yoga, and meditation along with conventional medicine, yet there was little research available about them. Also, many conventional medical practitioners had little to no experience with these modalities, how they would affect treatment, or if they were contraindicated.
The grant funded two programs, student development and faculty development. Said Benn, “We felt that, no matter how much teaching we – myself, Sara, Suzie Zick, and others – could do in the [traditional medical] curriculum, we wouldn’t be able to reach all the schools in order for them to understand what needed to occur in integrative medicine. Bringing faculty on board who could have that understanding, they could then teach their departments or their students in their schools.” This was the beginning of the Faculty Scholar Program.
Grant restrictions originally required faculty to create a project that was educational in nature. Benn explained, “That could be a course – in the School of Public Health that’s 32 credit hours, or in the medical school that’s five or six hours – or could be targeted to residents, a few lectures, but it had to be educated related.” Once the funding from NIH was discontinued, that restriction lifted and faculty pursued what they wished. It also allowed Benn to open the program up to faculty doing research and clinical service. As an example, she said,
“For some faculty members it changed the trajectory of their research careers. Our most famous scholar was Barbara Fredrickson, who is the queen of positive psychology and President of the International Positive Psychology Association. Barb developed a research project on lovingkindness, published it, and is now researching lovingkindness versus mindfulness meditation and the effects on anxiety and depression. She’s finding that one may be more beneficial than the other and looking at how our physiological functioning is affected by one over the other. Before [the FSP] she wasn’t doing that kind of work.”
Faculty scholars meet one Friday a month. “We always have an evidence based presentation, they have readings they have to do, there are discussion questions on those readings,” Benn elaborated. “Then we have a practitioner who comes in, who teaches us, and we may have a patient of that practitioner who shares their experience of that practice and what it afforded them. The scholars present an update of their project, and then there is some free floating discussion. It’s a packed day, and the discussions tend to be focused more on the transformation of health care.”
“There is a new national board certification in integrative medicine that is recognized by conventional medical boards. This could create a stream of students and professionals seeking certification. While the Faculty Scholars Program currently does not qualify, it easily could. The decision to do that would be up to Benn’s successor. ”
Each day has a focus; cancer, cardiovascular, chronic pain, and mental health, to name a few. Benn invites a presenter to talk about a given topic, and collects research articles and data about integrative medicine on that particular topic for the day’s schedule.
There are usually anywhere from 10 to 15 scholars a year coming from all over the University. Benn points to that as one of the accomplishments of the program. “Faculty have an opportunity across campuses and disciplines to learn from each other. Ours is very broad: art, music, business, engineering.” Some years they’ve also had faculty from other institutions, such as Eastern Michigan University and St. Joe’s Hospital.
As far as projects go, they vary. A pharmacy faculty member mimicked the medical school program and had her pharmacology students visit alternative practitioners in the community to develop familiarity with non-pharmacological options for care. A math professor distracted his students from their math anxiety by having them solve real world issues, such as calculating the glycemic index for foods they ate.
Then there is Sean Ahlquist, a Professor at the Taubman School of Architecture and Urban Planning. His research is on tactile and interactive environments. He also has a daughter with autism. His project united both of those areas, constructing a positive view of mental health. He created a video of his daughter titled Every Day We Look to Define Mental Health on Ara’s Terms. From that video, and with the support of Benn and his peers in the program, he developed a workshop for parents to construct a mindful view of the mental well-being of their autistic child. The workshops ran in the fall of 2015 for the first time.
Discussions, class time, and the year-long structure create what many scholars call the best part of the class: community. Michael Rice, M.D., Inpatient Medical Director of Gastroenterology, came to the program because “50% of inflammatory bowel patients use integrative medicine. I wanted to better understand for myself, for patients, and to incorporate [it] in [my] practice.” Rice, who went through the FSP with Ahlquist, says he was surprised by the camaraderie of the group. “It was a group of phenomenal people. [I] looked forward to spending time with them. [They were a] sounding board and inspired me.” Baylin concurred, “I was looking forward to that day.”
Hank Greenspan, a psychologist and playwright in the Residential College said, “It was a chance to talk across disciplines, to create a common language. People tend to talk in a certain language and style of work; professionally, [it was] an intercultural exchange.” Quyen Epstein-Ngo, of the Institute of Research on Women and Gender, said she went through a “withdrawal” at the end.
Benn points to a growing recognition among the medical profession of the importance of wellness “not only for their patients, but for themselves.” The program is a professional renewal of faculty, a “nurturing of faculty,” a quality that often falls by the wayside in the high pressured, achievement oriented University community. Many are so burnt out, according to Benn, or bored, or contemplating leaving academia. The monthly format “allows for deep work. I would say there is a therapeutic element; unexpected for them but [not] for myself. It is what will occur when you are a small group over time, talking about your own personal professional beliefs and views; you are also having these experiences (class visits and demonstrations).”
By allowing faculty to become students, they are given the permission all students have: to be curious, to inquire, to evaluate and reevaluate, to err, to test theories, and see how well they work, not just from a base of theory, but with experiential knowledge as well. The program creates an open, supportive space to learn, design, and play with new ideas, innovations, and cross fertilizations, then apply them into projects.
Baylin is one of the many faculty who has had her professional life reinvigorated. Jane Dutton is another. A distinguished Professor of Business Administration and Psychology, Dutton credits the program with giving her the courage and facts to pursue what she wanted to professionally 15 years ago.
Dutton’s interest was in rethinking management in the business world, how workplaces affect people’s health and how workplace design affects human flourishing. The research she was exposed to “fired her up to explore” what eventually became the University’s Center for Positive Organizations, a part of the Business School. She calls the program one of “the most transformative educational experiences I ever had, the most pivotal important intervention in [my] career.”
Baylin credits Benn with making it work so well. “Everything is consistent with the program, not just the talk – the food, the setting. I love the work Rita does and the people involved.” Dutton added, “Part of the magic [is the] safe and welcoming learning space. Able to handle conflict, able to handle vulnerability. We felt known as a person, could take risks, and authentically show up as you were.”
There is another, subtler aspect to supporting and nurturing faculty. When many of us reference “the University” or “the Medical School,” we may mean the physical location, but often we mean the institution and the culture, both of which are represented by the people in that culture. Our interactions with those people affect our understanding and perception of the institution itself. Think for a moment: what are your interactions and experiences like when you are overwhelmed or stressed out? How does that differ when you feel supported, engaged, and inspired? Nurturing faculty to bring out their best selves changes the face of the institution that patients, students, and the community interact with regularly.
With elated reviews, professional transformations, inter-professional connections, and innovative research, replication and expansion of the Faculty Scholar Program would seem obvious. However, that is not the case. While the start-up costs and first five years were covered by the NIH grant, and the next three by the Esperance Family Foundation, during the past seven years they have had to search for money.
Faculty who attend pay tuition, which usually comes from their department. Some faculty have paid themselves. Funding within the University is a topic of its own, but in general, faculty are encouraged to find grants to support their projects. In the medical school, research receives funds but not education, at least not directly. To receive money once a grant has been given, it is channeled through the department to faculty. The FSP is education focused and cross disciplinary, so while it has found a home in Family Medicine, it belongs to the entire medical school. It is an ongoing program, which most foundations have no interest in, instead wanting the institution to take up the costs.
Added to this is Benn’s position as adjunct faculty, a change she made seven years ago to teach at Dr. Andrew Weil’s Arizona Center for Integrative Medicine. After a year of flying between the program in Ann Arbor and Tucson, she decided to remain in Ann Arbor as an adjunct.
Adjunct faculty have a different role in the university hierarchy than permanent faculty. They participate less administratively, and therefore, as Benn says “the University has less obligation to them.” They are also limited in access to funding opportunities. These factors combined with those listed above have hampered the project financially, and there is a precedent for failure. The University of Washington had a similar program that ran for three years, with staff trained by Benn, but then “the staff left and the funding left, so there wasn’t a champion to keep it going.”
Costs for the program are a short list: Benn’s salary from the Department of Family Medicine, copies to give to the faculty scholars, food for their meals, renting the classroom, payment to the visiting practitioners (although many give their time unpaid). Benn herself does all of the research collection, email coordination, recruitment, arranges the food, the location, the practitioner visits, as well as the teaching. A small of amount of money is paid to the Department of Family Medicine to keep track of the financials – has tuition been paid, the food vendors, the practitioners?
When asked what the program needed to be sustainable, Benn said that an extra $10,000 aside from tuitions would cover it. Similar programs nationally cost $5,000 to $15,000, according to her, whereas the University charges faculty and their departments $2,250 to take the program. If they were to raise the cost to between $3,000 and $3,500, Benn believes it would be sustainable locally, although she added, “donors are welcome.”
Northwestern University implemented the program last year and is continuing it this year with assistance from two of Benn’s graduates. Benn is currently training an individual at Beaumont Hospital in metropolitan Detroit to run a similar program there, and recent changes in the world of medicine could assist the program. There is a new national board certification in integrative medicine that is recognized by conventional medical boards. This could create a stream of students and professionals seeking certification. While the FSP currently does not qualify, it easily could. The decision to do that would be up to Benn’s successor.
When I originally spoke to Benn in 2015, there was no successor in sight and the FSP’s demise appeared certain. Benn had searched for a successor and had just had a potential candidate bow out due to too many commitments and the funding difficulty remained. When I contacted her again in the middle of 2016, she emailed that she was in discussions with her department, Family Medicine.
In October 2016, Dr. Sara Warber retired. Her leaving proved a catalyst to decision-making and made apparent that if the program was not to disappear, it would need leaders. Suzie Zick, Naturopathic Doctor and M.P.H., and Jill Schneiderhan, M.D., stepped forward. Zick is a researcher, Schneiderhan a clinician and a graduate of the program. Current plans are for the two to co-direct for the next five years and bring it more firmly under the umbrella of Integrative Family Medicine.
Benn says there has been “a recognition of the core value of integrative medicine to family medicine for patients. We have shown the value in the last 15 years and made our case.” The question is, will that case be strong enough to garner funding? Will it become fully funded as it moves deeper within Family Medicine? Will it become absorbed in the total curriculum, giving faculty the support for developing new programs and initiatives that could benefit students and patients? Or will it disappear in five years, a legacy unfulfilled?
For Benn, she says this may be her last year or there may be one or two more. She is very involved with Michigan Collaborative for Mindfulness in Education (MC4ME), a group working on bringing mindfulness into elementary education (See the interview with Mary Spence in issue #62, available on CWJ’s archive online), and should hear soon about another grant, this time with Suzie Zick, to train professionals in integrative oncology. She would like to get the program into more universities and hospitals and leave a legacy of integrative health. And then there is Alice, her granddaughter, who recently moved to Ann Arbor while her mother does a fellowship at the medical school and her father finishes his Ph.D. Having Alice local “thrills me!” says Benn, especially since her other children live in California and New York.
“With elated reviews, professional transformations, inter-professional connections, and innovative research, replication and expansion of the Faculty Scholar Program would seem obvious. However, that is not the case.”
The final class offered to the faculty scholars is optional. Its title is “Leadership and Systems Change.” Benn stated, “I think what can also transform the system is when the leadership of that system has their own personal experience. We have the data and the data supports [a] benefit of quality of life for these modalities. We think that policy change occurs because of data but it doesn’t, it occurs because of personal experience and persuasion.” After 15 years, 150 scholars, numerous programs designed and implemented and countless classes, Rita Benn has persuaded and inspired many of her colleagues of the value of integrative health for all, especially for those who teach. For it to flourish and grow, nourished and funded, and continue to benefit faculty, patients, and students in the future is up to her successors and the University.
To view a list of scholars and their projects go to www.med.umich.edu/umim/education/um-scholars.html. Rita Benn can be contacted at ritabenn@umich.edu.

























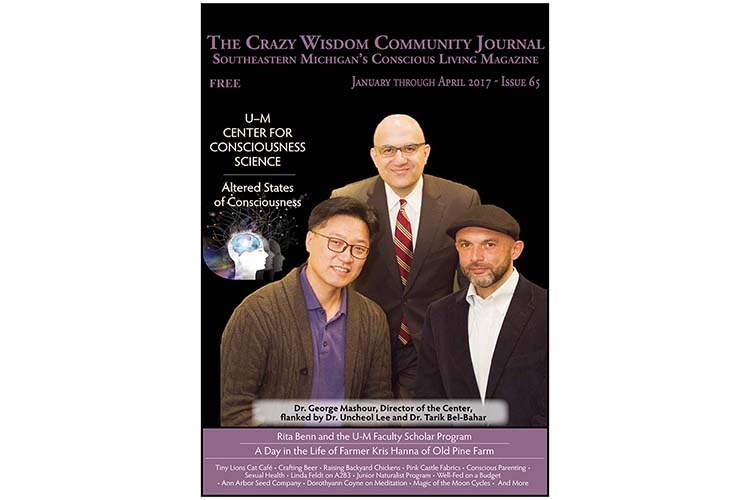



The Center for Consciousness Science at the U-M Medical School was inaugurated in June 2014 by its Founder and Executive Director, Dr. George Mashour. That was around the same time that Dr. Tarik Bel-Bahar arrived in Ann Arbor. We were approached by Bel-Bahar in mid-2015, who suggested that CCS’s mission and activities might be ripe for a story in the CW Journal. We agreed. So what follows is an interview with Dr. Bel-Bahar, about the Center and its work. For long-time Crazy Wisdom Journal readers, this is a “must-read” about exciting work on the frontiers of consciousness research being done right here in Ann Arbor, right at the University, in the Medical School, no less.