By Meghan Marshall
Anyone who’s ever had a “gut feeling” or felt the stomach-sinking effect of bad news probably believes in some kind of connection between the brain and the gut. These people would be right. However, the strong bidirectional communication between the brain and the digestive system is much more complex and intertwined than most people realize.
Bidirectional means that there are messages being sent both from the brain to the digestive system, and from the digestive system to the brain. The digestive system even has its own nervous system—the enteric nervous system.
The brain sends nerve signals, which are either carried out by the parasympathetic nervous system or the sympathetic nervous system. The parasympathetic nervous system is known as the “rest and digest” system, while the sympathetic nervous system is what responds during dangerous or stressful conditions. Consequently, when the parasympathetic nervous system is responding, gut function is stimulated while the sympathetic nervous system inhibits gut function.
These signals are sent using nerves, hormones, and inflammatory molecules. The vagus nerve is one of the key components of this brain-gut connection. The connection of the vagus nerve between the gut and the brain can influence factors like appetite, food intake, pain, mood, and more. Interestingly, most of the signals sent via the vagus nerve go from the digestive system to the brain; for example, when the stomach is empty, ghrelin is released from the gut to stimulate feelings of hunger from the brain. The information generated in the gut that reaches the brain is then interpreted by the brain and sent back to the gut in order to adjust its functions.
Knowing about this strong and intimate connection between the gut and the brain, it only makes sense that emotions, or a certain state of mind, can considerably impact digestive functions. Particular emotions can even be a predictor of certain diagnoses, like irritable bowel syndrome or chronic constipation. How can this be possible? Well, as mentioned, the body reacts via different systems depending on the present situation. When stress or danger is signaled, the sympathetic nervous system responds, moving blood away from the digestive system to help negate the threat (i.e. bringing blood to the muscles so you can run away), inhibiting the vagus nerve and slowing digestion. The hypothalamus in the brain releases a molecule called corticotropin releasing factor (CRF), generating a gastrointestinal stress response and also releasing the stress molecule cortisol.
Read related article: Why Your Gut Won’t Heal – And What You Can Do About It
During very high-stress or anxiety-inducing situations, the gut signals are felt more sensitively, which is what can lead to an immediate response of diarrhea or even vomiting during these types of situations.
This response is very helpful in life threatening situations. However, it becomes problematic when this response is chronic; common in our high-stress, demanding lifestyles nowadays. With persistent unpleasant emotions—as in someone with an anxiety disorder—this can lead to changes in the enteric nervous system over time. These changes can induce continual, increased gut sensitivity and lead to symptoms like bloating, stomach pains, or constipation. This dysregulation in the digestive system can eventually lead to diagnoses like IBS, indigestion, or chronic constipation or diarrhea. Unfortunately, each of these can be a “catch all” diagnosis when physicians can’t seem to find a physical explanation for the cause of these symptoms. Treatments for these conditions are usually aimed at minimizing symptoms instead of correcting the root cause for the dysregulation, and relief from the symptoms can be hard to come by even with these therapies. New studies are now being conducted on the effectiveness of psychotherapies like cognitive behavioral therapy, mindfulness, and hypnotherapy for IBS and similar conditions with promising results.
Stress isn’t the only emotion that can have an impact on the digestive system, however. Depression, sadness, and hopelessness can result in a decrease in peristalsis, which are the wave-like contractions along the digestive system that help to move the food through the intestines, possibly causing constipation. Anger and aggression can trigger the contractions in the lower intestine.
Furthermore, your body has the ability to store responses and memories of a traumatic or stressful event, which can elicit reactions after the event occurred, even years later. Childhood and even generational stress can cause a predisposition to the gut overreacting to stressors, leading to gut-related symptoms.
On the reverse side, dysregulation in the gut can also have a negative impact on a person’s mental and emotional state. One type of dysregulation could be the makeup of one’s microbiome, which is the name for the trillions of microorganisms that populate the digestive tract. The activity in the brain or state of mind can influence the microbiome, and the microbiome can reinforce emotions and even prolong them. Not surprisingly, the microbiome has the ability to also influence risk for digestive diseases. Some of the non-beneficial or harmful microbes are able to increase their numbers with the metabolites that result from stress. This imbalance of “bad” bacteria in relation to the beneficial bacteria is called dysbiosis. Dysbiosis can also lead to undesired gut-related symptoms.
Studies are even starting to show the association between neurodegenerative diseases and the gut. Parkinson’s disease, a progressive neurodegenerative disease, may be one example of this. Some recent studies have found that even before characteristic Parkinson’s symptoms materialize, the enteric nervous system goes through the typical Parkinson’s nerve degeneration and is accompanied by a change in the gut microbiome.
With all of this evidence contributing to clear proof that the mind and the digestive system are strongly interconnected, what should you do with this information?
One recommendation is to avoid eating whenever you’re experiencing high, short-term stress. The body’s focus won’t be on digestion during this time, which can lead to acute gut-symptoms like stomach pain and bloating.
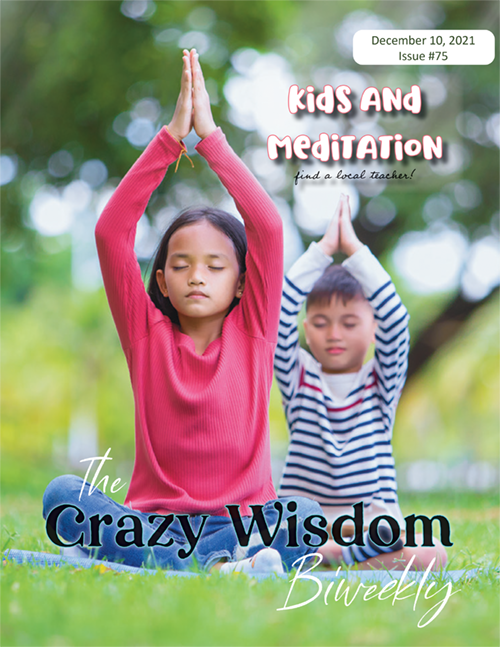
For someone who’s chronically stressed or overwhelmed, therapies aimed at relaxing the mind and body can be beneficial. This could include yoga, meditation, walking, or spending time in nature.
In regard to supporting the microbiome, fermented foods are ideal. Some recommended sources are kimchi, miso, sauerkraut, and unsweetened yogurt or kefir. While food sources are optimal, supplemental probiotics can be an alternative. However, desired results can vary depending on probiotic strain, so it is recommended to begin these under the supervision of a qualified medical professional. A healthy diet with plenty of fruits, vegetables, and whole grains is also favorable for gut health and supporting the microbiome. Avoiding antibiotic overuse and not purchasing antibiotic soaps or household products can further benefit the microbiome and help to reduce the risk of antibiotic-resistant bacteria.
Being aware of this impactful gut-brain interconnection can help lead you to a happier, healthier life.
Meghan Marshall is a Registered Dietitian with a master’s degree in Nutrition and Functional Medicine. Meghan currently works as both a clinical and community dietitian, and is the owner of Black Moon Nutrition + Wellness. She is the creator of and writer for the new blog, Black Moon Nutrition Blog blackmoonnutritionblog.com.





























mcdonald lives in White Lake, with his wife, Stephanie, their three kids, a dog, many cats, and two ferrets. Stephanie is deeply involved in running the business and website, and they “keep doing a little bit better every year.” mcdonald is a very winning fellow – chatty, engaging, tangential, lively, casual. He is a man who has developed a deep love for plants, and it shows. “Plants are awesome,” he says. They are an “intermediary” between nature and humanity.