By Meghan Marshall
Bacteria and viruses have always gotten a bad reputation in our modern society, but these microscopic microorganisms are essential to human life and can quite literally be a key aspect to our optimal health. In fact, trillions of bacteria, viruses, fungi, and other microbes live all over our bodies, with the largest concentration in our intestines.
Each person has their own unique microbiome that is influenced by multiple factors including DNA, external environment, diet, mental health, and more. However, our microbiome is not set in stone at birth. It can change during different stages of our lives, such as with a large change in diet habits, the use of antibiotics, or even with illnesses like Parkinson’s disease.
The question most people likely have when finding out they share their body with trillions of tiny microbes is: why? Truthfully, experts are still in the process of finding out all of the different functions of the microbiota but there are some functions researchers and scientists already know for sure. A large part of the gut microbiome’s purpose is to help us digest and metabolize our food properly, in addition to drug metabolism, keeping pathogenic microorganism numbers in check, maintaining the intestinal barrier, synthesizing certain vitamins, and more. The microbiome is even a key factor in the bidirectional communication between the central nervous system and the digestive system.
The organisms in the microbiome mostly utilize carbohydrates, and in the case of fiber, which is indigestible, it is fermented in the intestines where beneficial by-products are then produced that are important to digestive and general health. These by-products are called short-chain fatty acids (SCFAs) and can decrease inflammation and can even reduce one’s risk for illnesses like Inflammatory Bowel Disease (IBD) or certain cancers. These SCFAs may even be beneficial for the central nervous system, thanks to the gut-brain axis. The microbiome has also been shown to assist with the breakdown and utilization of essential nutrients, like polyphenols, from foods.
The microbiome is also extremely important to the immune system. The microbes that make up the gut microbiome have been shown to be significant to the production of cytokines and T cells as well as the regulation and proper response of the immune system. In addition, the gut microbiome has the large responsibility of keeping pathogenic microbes, the microbes that can be harmful, in check. This is done both with the beneficial microbes being in a larger quantity than the pathogens and sustaining these higher numbers, as well as the beneficial microbes’ ability to stimulate the immune response against pathogenic strains. The digestive system is so vital to our body’s immunity that it even has its own lymphoid tissue, the gut-associated lymphoid tissue (GALT) which happens to be the largest mass of lymphoid tissue in the body.
Clearly, the trillions of tiny microbes in our digestive system are extremely important to our health and wellness. So, what happens if there is a disruption, or dysbiosis, in the microbiome? Generally, we can have smaller amounts of the ‘bad’ pathogens in our digestive system without it being an issue and, in fact, it’s totally normal. The problem can happen when they start to grow in number, unchecked. If the healthy microbiome gets disrupted and numbers of beneficial microbes decline, opportunistic pathogens can increase and become the dominant strains. Dysbiosis can also include a low diversity of different types of microbes in the gut. Unfortunately, there are multiple different ways the microbiome can become disrupted, including the use or overuse of antibiotics, mental or physical stress, medications, and even poor dental hygiene. Diet is also another common cause of dysbiosis, specifically with a high intake of meat and added sugars and a low intake of fiber and vegetables.
Although a dysbiotic gut microbiome has been found in conjunction with chronic illness, the exact relationship between the two is unknown. That being said, there are many different diseases that have some type of association with a disrupted microbiome including Multiple Sclerosis, Alzheimer’s Disease (AD), Parkinson’s Disease (PD), autism, metabolic disorders like type 2 diabetes and obesity, psoriatic arthritis, allergies, autoimmune diseases, irritable bowel syndrome, inflammatory bowel disease, and more. Parkinson’s disease, a well-known disease of the central nervous system, often includes gastrointestinal symptoms, and when fecal samples of PD patients were taken, it was found they had a decreased concentration of SCFAs and markers of dysbiosis with the possibility there may be certain specific microbes that are associated with this disease. In AD, a dysbiotic microbiome has been shown to have some correlation with the progression of the disease. Some studies have even shown that in depression models, SCFAs are decreased.
As mentioned, the exact role of dysbiosis in many common chronic diseases is unknown, and whether the dysbiosis is a side effect of the disease or a predisposing factor to developing the disease needs further exploration.
With the obvious need to support the gut microbiome to help reduce the risk of disease and aim for optimal health, what actions can be taken to do this?
One of the easiest ways to support your microbiome is to eat a diet that supports your beneficial bacteria, which includes both prebiotic and probiotic elements. The Mediterranean diet is one of the most widely studied diets with a proven benefit to health. This diet contains many of the microbiome-supporting factors, including a high intake of whole fruits and vegetables, whole grains, plant proteins and healthy fats while limiting intake of animal proteins, added sugars and refined grains. Another supportive measure is to eat naturally probiotic foods like low-sugar yogurt, kimchi, sauerkraut, kefir, miso, and tempeh. Prebiotic foods are high in certain types of fiber and are found in foods like beans and legumes, whole grains, fruits and vegetables such as onions, garlic, asparagus, barely ripe bananas, and Jerusalem artichokes.
Read related article: A Barefoot Approach to Wellness
However, a healthy diet is only part of the puzzle for supporting the microbiome. Trying to reduce stress or implementing stress-reduction techniques like meditation or mindfulness, getting regular adequate sleep, and engaging in regular physical activity are extremely important as well.
Probiotics are currently very popular and although they definitely have a place in optimizing the microbiome, different probiotic strains have different purposes and many probiotic products on the market don't actually contain what they claim and may even contain additional ingredients not listed. For these reasons, it’s best to work with a medical practitioner before supplementing with probiotics.
The microbiome can also be supported by limiting use of antibiotics except when truly necessary and avoiding the use of antibacterial products and soaps.
The gut microbiome is so wonderfully complex and even with all that is already known about the microbiome, research has only scratched the surface. What is known is that a healthy microbiome can help you lead a healthy life and reduce your chances of illness and disease, so make sure to take care of yours!
Meghan Marshall is a Registered Dietician with a master’s degree in Nutrition and Functional Medicine. Meghan currently works as both a clinical and community dietician and is the owner of Black Moon Nutrition + Wellness. She is the creator and writer for Black Moon Nutrition at blackmoonnutritionblog.com.












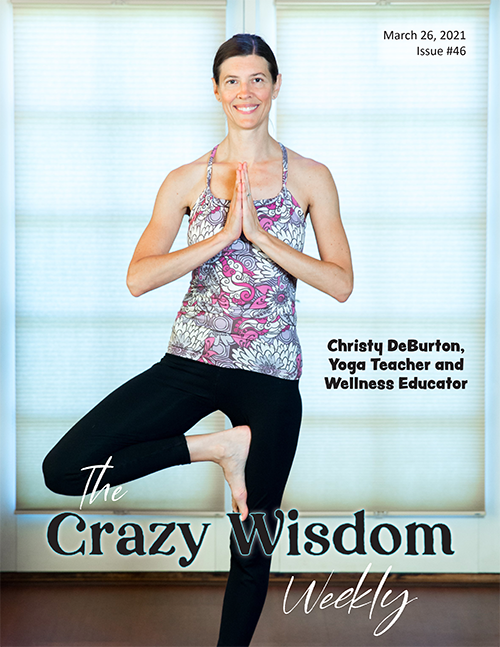







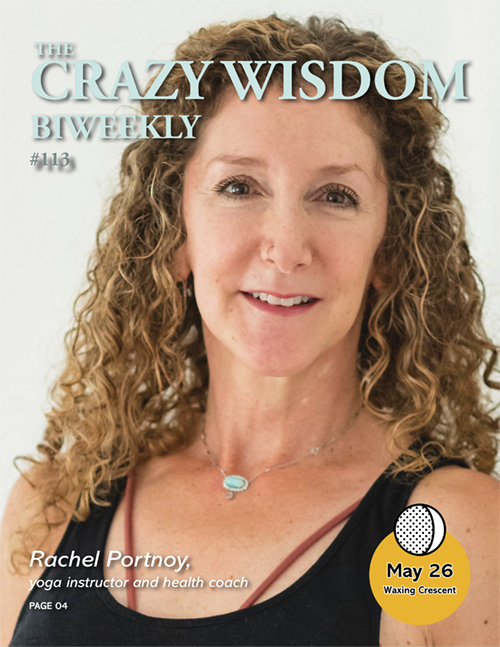













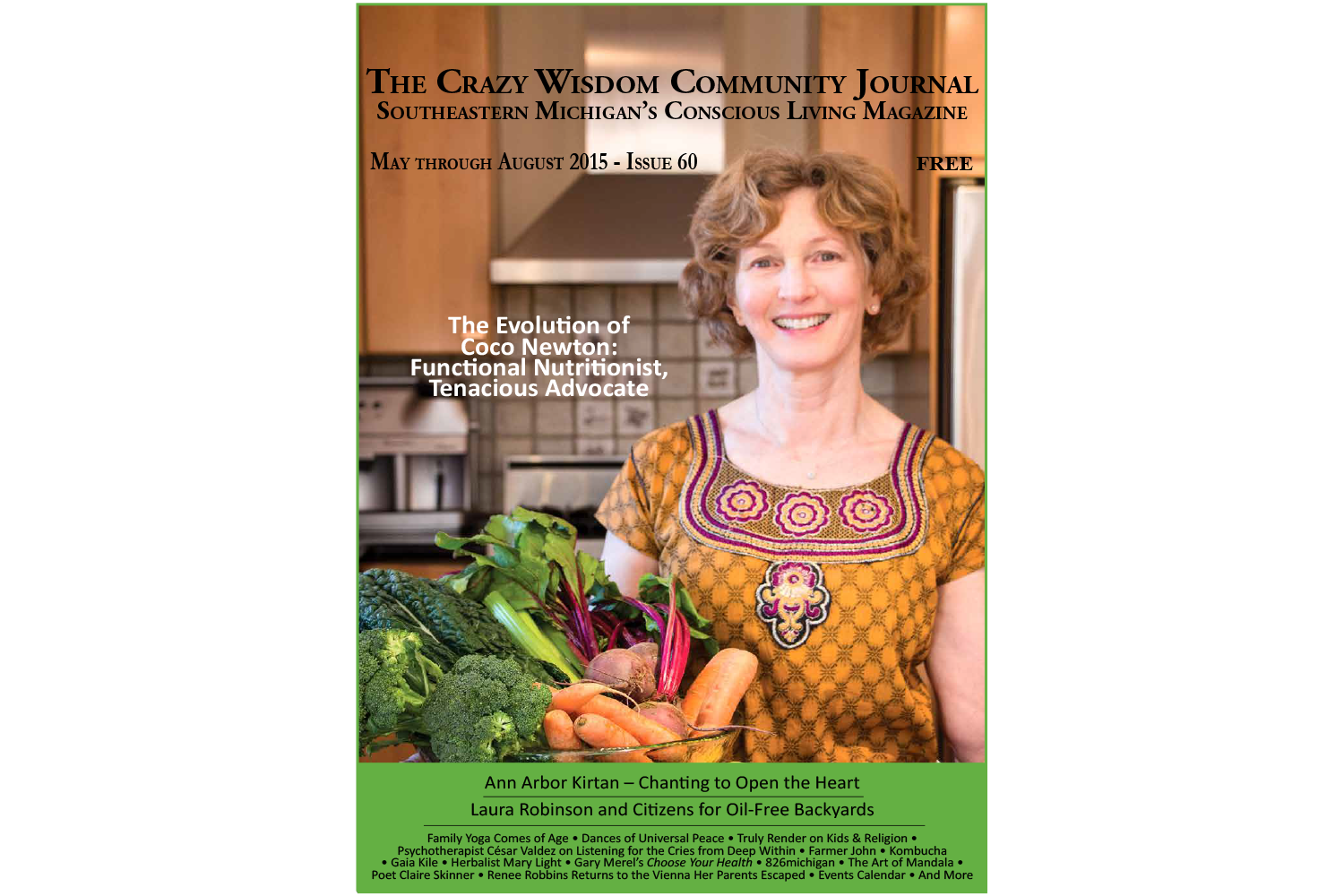



As an accomplished athlete, real-food advocate, and wellness guru, Hoffman seeks to serve the whole person with her unique fitness philosophy.