By Kirsten Mowrey
Allison Mitchinson walks through the Veterans Hospital in Ann Arbor as an old hand. Sliding around groups, easing her way through the busy hallways, she confidently guides me until we come to a nondescript door that leads to an inner office area. Here, at her desk, “whole person treatment” is taking its latest step in a long journey. Mitchinson, a licensed massage therapist, creates integrative care within the hospital environment. She and two colleagues are using their expertise to help local veterans address pain and health issues. They are also publishing research about their work.
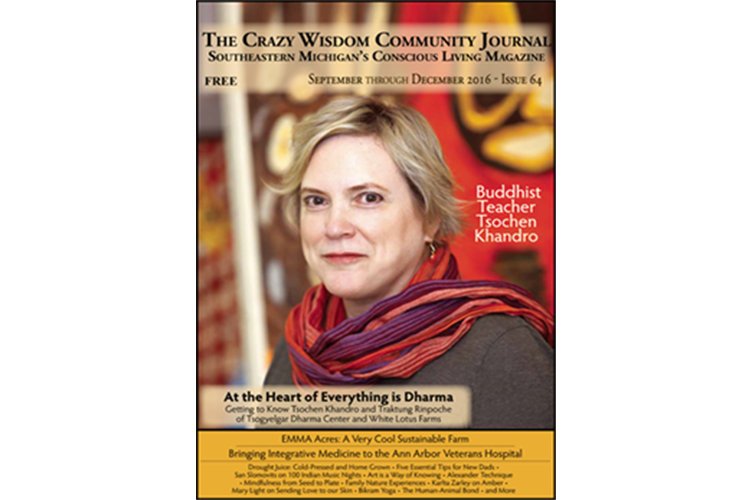
Integrative medicine, in the forms of massage, acupuncture, spinal manipulation, and energy work, has been growing in America since the early 1970s under various names and guises like complementary care and alternative medicine (CAM), and has been hugely successful in the private sector. Integrative therapies run a parallel course to traditional medical care, with patients crisscrossing into each system, but professional cross-pollination has been minimal. According to Dr. Rita Benn, Director of the University of Michigan’s Faculty Scholars Program, there are around 60 universities that have small programs working with integrative care, mostly because of champions within each system committed to using it.
“We had very supportive management,” said Mitchinson, explaining how integrative medicine came to the VA administrative leadership and grant support provided the initial push. She explained:
I was working in the health services research and development group, finishing up going to [massage] school, and found out Dr. Hinshaw, who was chief of staff here at the time, was doing a pilot study on massage therapy. I wrote and asked if they needed any help, and next thing I know, I was involved with it. That pilot study in 2000 was the predecessor to [a published] study. I wrote the grant for that in 2001 with Dr. Hinshaw.
The study researched postoperative pain management following cardiac surgery, using massage as an adjunct (assisting) therapy. It was the largest random controlled study using massage at the time. The conclusion? “Massage is an effective and safe adjuvant therapy for the relief of acute postoperative pain in patients undergoing major operations.
“It is unprecedented: a large traditional health system reaching out to tap into the local wealth of integrative therapies, to better provide for the needs of their patients.”
Mitchinson continued in a level voice, pausing to adjust her glasses: “Originally, there were two proposals, one for a massage therapy program in palliative care and one for pain management. I was working with Dr. Hinshaw to make the pain management proposal and the VISN proposal.” VISN is short for Veterans Integrative Service Network. The nation is broken up into 22 regions, or VISNs, with each area meeting required dictates for care. Locally, our VISN includes the Lower Peninsula of Michigan, Ohio, and Indiana. “We were told: we’re not going to fund both of these but we’d like you to do both of these. So that was how the whole thing started. The VISN’s acceptance of the proposal and willingness to fund it was a direct effect of that study — [it had] shown [massage] was effective.” The study was published in 2007 in the Archives of Surgery, the same year Mitchinson’s grant for massage therapy was accepted by the VA. Her massage therapy position began in 2008.
Her colleague, Dr. Paul Moga, arrived in 2007. With two professionals on board, integrative care had arrived in the VA Ann Arbor Healthcare System. A compact, bearded man, his demeanor is quiet and attentive. “I started life as D.O. [Doctor of Osteopathy] and went back to school to do graduate work in biomechanics. I gravitated from family practice to musculoskeletal in the late 90’s, and did occupational medicine at Detroit Medical Center for the city’s police and fire fighters.” After that he began his fellowship at the VA, doing manual medicine part-time at the VA hospital. Manual medicine is the use of palpation and directed techniques to aid in the diagnosis and treatment of musculoskeletal disorders. If a patient has pain with lifting, for example, a clinician may touch the areas affected, move a joint through range of motion, and use body weight or pressure to improve function. He explained, “I was finishing my year, my boss said, ‘How’d you like to stay?’ and I said, ‘OK.’ I started doing more manual medicine, started the clinic, and taking on additional responsibilities.”
For years Dr. Moga and Allison Mitchinson were it for the clinic, until Nurse Nancy McKlaren arrived in 2015. McKlaren provides Healing Touch, an energy therapy where practitioners consciously use their hands in a heart-centered, intentional way to support and facilitate health and healing. “I’ve had men who sat right where you are who said, ‘I think it’s a bunch of hogwash and I think it’s stupid, but the doctor asked me to do it, so I’m going to do it,’” related McKlaren. “And then when I’m done, they sit up off the table and they are like, ‘Wow, that was intense,’ and at that point they buy right into it. ‘I’m coming next week.’ Experience speaks louder than [their] belief system.”
Taking a moment to adjust her long dark hair, she continued:
I think the one that surprised me the most was the one who was nearly 70. He comes in, dressed like a motorcycle biker, big long beard, I just kinda looked at him and [thought], This guy is gonna walk out of here and say it’s hooey. I got done and he says, ‘I don’t know if it helped me, but I’m going to come back in a week.’ He came for four or five sessions. He was one of my hypertensives and had a significant drop in his blood pressure. Another case, she was around 50, migraines, multiple trips to the E.R. over the past year, her primary care was trying everything: acute pain meds, as well as long acting meds for migraines, MRIs, CT scans — couldn’t keep migraines under control. [Her doctor] suggested that she get massage and Healing Touch, back to back. She’d get Healing Touch, go home, and within an hour, get massage. We had four treatments like that and she didn’t have a migraine after. After a year of emergency room visits!
Receiving care from these practitioners follows a pattern similar to their allopathic colleagues: consultation, evaluation, treatment, and a treatment plan for the veteran. Integrative practitioner appointments are handled like any other practitioner when it comes to scheduling and referrals. The recipients draw from a wide area: “Some from Kalamazoo, from northern Indiana. One guy came from Alpena area and one from the U.P. and he’s moved here, because the people in [VISN] 12 didn’t give him what he needed!” chuckled Moga. “Battle Creek facility doesn’t have this modality, they don’t even have fee-based for this modality, so in the state, this place is the place to come for alternative medicine in the VA.”
The desire for these services, however, has far outstripped the offering. “The truth is I haven’t been able to accept a new consult for chronic pain since 2009,” admitted Mitchinson, when I asked her about her patient load. According to the American Massage Therapy Association, the average massage therapist sees 15 people a week, for a total of 60 sessions a month. “They need a referral by grapevine, curbside,” said Moga. “At one point I had an official consult form but I was just inundated, and my boss said you need to take care of who you have on board, so I stopped.”
For some hospitals that consider adding massage, concerns about high demand have outweighed Mitchinson’s research demonstrating efficacy of treatment. In an alternative therapy health medicine journal, the Salt Lake City VA admits to not adding massage “because hospital administrators were concerned that the clinic would be overwhelmed with requests.”
In Ann Arbor, high demand and limited access caused the Ann Arbor VA to seek a solution outside the system, referring veterans to private therapists. It is unprecedented: a large traditional health system reaching out to tap into the local wealth of integrative therapies, to better provide for the needs of their patients. Choosing to make this move, with no institutional history to guide them, the Ann Arbor VA shows a deep commitment to the needs of their patients.
Non-VA providers are required to submit treatment notes and bills for all services, and each prescription requires a report and is only for limited duration. Dr. Moga reviews each request:
Referrals have to be aligned with primary care thinking. I try to educate them [primary care doctors] on the caveats when we are looking at any of those modalities. I researched looking at the big private sector insurers. What CAM things do they cover? Some acupuncture, not many massage, chiropractic different numbers. So here’s what we did: we will go beyond what the private sector insurers offer their members. We’ll take 26 visits a year for primary care modality, 13 visits a year for the secondary, which, when you total them, means you have a care modality every week and a half, which I think is really impressive.
““Experience speaks louder than [their] belief system.””
Impressive, yet institutional elements prevent expansion. Structurally, the VA’s system for care requires only one manual medicine (D.O. or chiropractor) practitioner per region. For years, Ann Arbor was in VISN 11, which included the Lower Peninsula of Michigan, most of Indiana, and about one-third of Illinois. Dr. Moga informed me there was a slice of northwestern Ohio in there, too. Currently Ann Arbor is VISN 10, which removes Illinois but adds Ohio and some of Kentucky. That’s an immense area for one individual. There are no requirements for other modalities. Massage faces a very knotty difficulty: Congress. Because there is no official designation of massage therapist within the VA system, the only way to add it is with Congressional approval. I asked if this is VA policy, or a quirk of management, or historical law. Mitchinson replied, “No, just the way the legal system works. They just can’t willy-nilly decide they are going to have a job classification without the approval of Congress. It’s the same for any job, it’s not particular to massage therapy. I don’t even think it’s particular to the VA, it’s federal.” Mitchinson was hired as a research science health specialist and now is listed as a program specialist, not massage therapist.
Another challenge? Recall the nondescript door that I mentioned at the beginning? It leads to where Mitchinson massages her patients — in an office area crowded with cubicles, printers, and clinicians. She does not have a treatment room. Mitchinson has a cubicle desk here, one of four desks in a square unit, her walls covered with photographs and mementos. The whole unit is only about 12 feet deep. Dr. Moga and Nancy McKlaren, located near primary care, have their own rooms with doors, treatment tables, and desks; each room is bigger than Mitchinson’s square unit. Inpatient massage is done in the room, but for her outpatient chronic pain patients, she takes her portable table, stored in the hallway, elsewhere.
“Elsewhere” is a ten minute journey away. If you’ve seen or driven by the VA hospital, you’ll note how long it is, its long brick walls stretching along Fuller Road. To get to Mitchinson’s outpatient room, we will walk the length of the building, plus additional winding corridors. Eventually, we are at the opposite side of the building from the main entrance. Here, in one of the treatment rooms, is where she sees her outpatient pain patients two afternoons a week. The room contains a sink, a treatment table with drawers below, and a few chairs. The atmosphere is distinctly clinical. Allison moves the furniture each time to create enough space to set up her table and massage her clients.
Finally, there are the veterans themselves. Veterans seeking care are more typical of hospital patients than the general population. Mitchinson explained:
I’ve done massages on so many people that most massage therapists wouldn’t even touch, they’d be too afraid. I just worked on this one guy this week, he had melanoma. He had these little tumors all over him. They sent him to me because he’s having neck pain and shoulder pain. He’d already had a surgical excision in his armpit, and here [indicates top of arm] and I think that’s why he was having the shoulder pain. Then he’d had four weeks of radiation with the arm torqued out like this [gestures], numerous little tumors, and three or four little melanomas [near surgical site]. This poor guy, he’s coming, he can barely walk, and to get to me, is a huge ordeal. He drove here, from Ypsi, this particular guy, but I have guys coming up from Ohio, 90 miles each way. You want it to be something for them, so you do whatever you can.
Despite all these hurdles, reception of this type of care has been extremely positive. While I could not interview individual veterans due to privacy policies, the Journal of Rehabilitation and Research Development paper that identified obstacles also cited veterans’ responses to massage. Researchers noted:
Participants reported an overwhelmingly positive response to the therapeutic massages, chiefly as a way to relieve pain but also to increase mobility and flexibility; promote relaxation; foster more restful sleep; and reduce anxiety, stress, depression, and fatigue. Some participants reported an initial increase in pain associated with the depth of the massage, but all felt the end result justified the experience. [A patient response was:] “She really works my muscles and it’s painful, but I always feel better before leaving.”
Other patient responses were: “It’s beautiful, they should have it for all veterans,” and “If I had my druthers, I’d be up here about every week.”
And: “I would like to see them be able to fund more massage therapists and manual medicine people because your body is connected from the tip of your toes to the top of the head and if one place is irradiated then its going to affect the rest of your body and it also affects your temperament.”
Meanwhile, the practitioners keep their focus on what they can do. Nancy McKlaren serves on the VA’s subcommittee for CAM modalities.
“I am 200% supportive of what Allison is doing,” said McKlaren. “In August [2015] we had an integrative training for nurses, offering training and a certificate in four different modalities. This is a grant that Allison got to bring more CAM into the hospital. 25 nurses, 12-13 from our extended care and 12-13 from ambulatory care. [We are] training nurses to do guided imagery, simple massage, acupressure, relaxation therapy techniques.”
Allison Mitchinson is reaching beyond her colleagues. “This VA services something like 50,000 veterans, you can’t hire enough massage therapists, so how do you get more touch into the system?” she asks. To that end, she has created a toolkit, a document with a DVD to educate nonprofessionals. “You get volunteers, you train family members, you get other care providers to do it. That’s part of the toolkit, we give them information on other ways.”
When not doing massage, Mitchinson writes grants for research. Since her 2001 study, she has conducted and published four more studies: one on massage integrated with veteran’s palliative care, two on perceptions of CAM within the VA (one local, one national), and one on the relationship between veterans and their massage therapists and how it affects their pain. She presented at the Massage Therapy Research Conference in May 2016.
The evolution these practitioners represent cannot be overstated. It is a new horizon for allopathic medicine to have massage, manipulation, and Healing Touch included in care, administered by staff members, and paid for by insurance (with the government as the insurance provider). Having integrative practitioners within the hospital environment and as colleagues expands our definition of “health” and “care.” As part of a veterans’ care plan, with practitioner’s notes part of the medical record, these modalities become a part of the spectrum of care, not separate. It offers, to quote one study from Complementary Therapies in Medicine, “...care that enhances healing by increasing the ‘capacity of the organism to heal itself.’”
Supporting the entire body, with its many feedback loops and integrated systems, may be the way to real health, for veterans and for ourselves.
Kirsten Mowrey, LMT, BCTMB, is a local body and energy medicine worker. This is her fourth major feature article for the Crazy Wisdom Journal.