Interview by Kirsten Mowrey
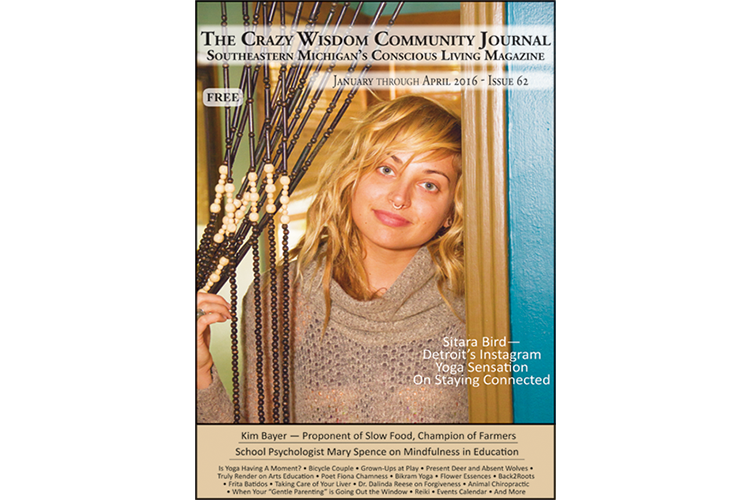
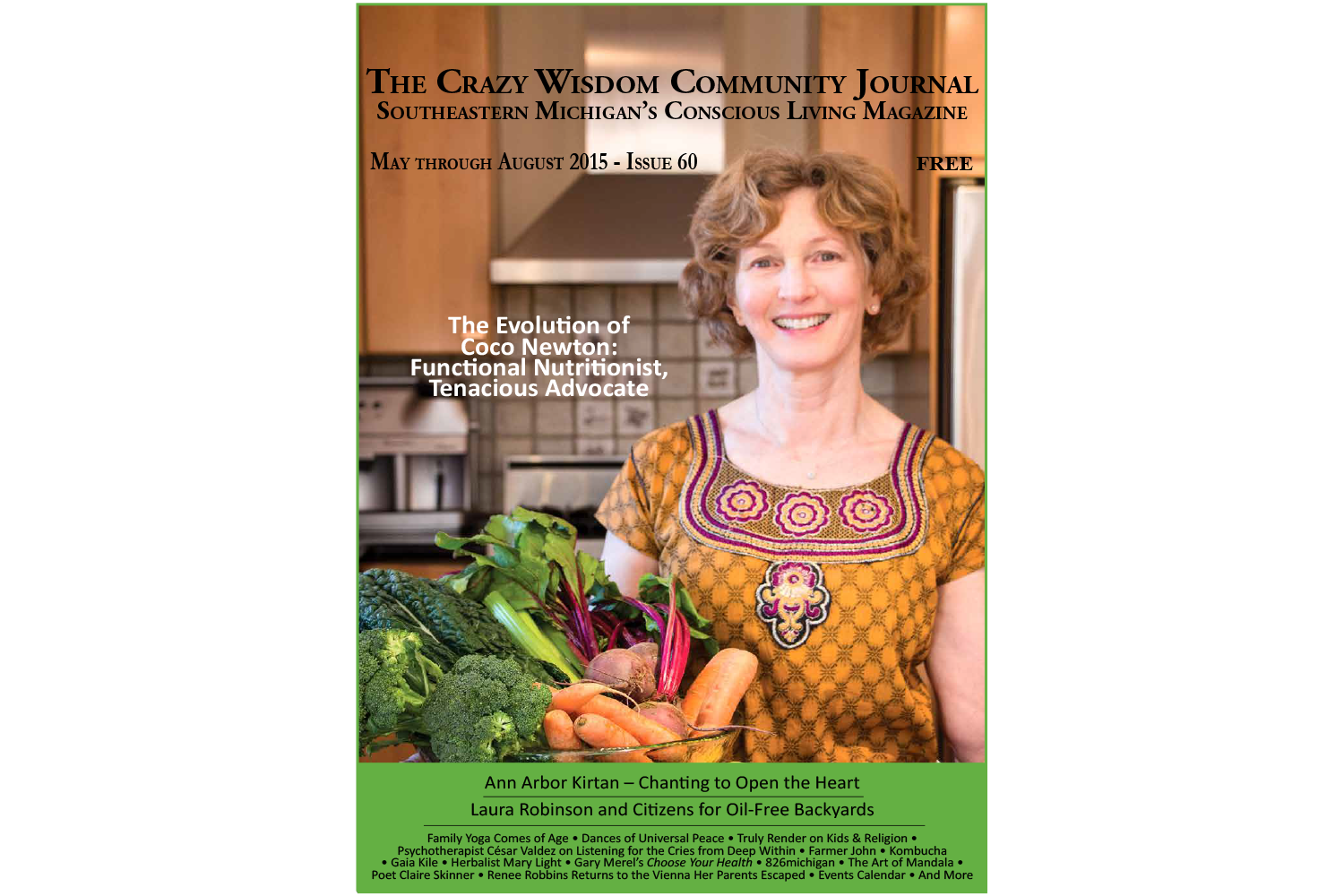
Photography by Linda Lawson
What follows is an extensive interview with Coco Newton, a leading functional nutritionist in our region, exploring her nutrition philosophy and personal story. We’re highlighting her in The Crazy Wisdom Journal because she has a fascinating story of slowly coming around to being integrative, at first coming from a hospital background and now working in private practice for many years. As she puts it, hers is a “whole eater” approach, incorporating extensive assessment and diagnostic tools. Because of this, she is utilized and respected by traditional doctors, chiropractors, osteopaths, and integrated doctors alike. Her work is not “alternative” or “complementary” per se, but perhaps upholds a new standard of care, one that has made her practice extremely successful.
Coco Newton is also well-known in this region as wife and partner to Roger Newton, the Ann Arbor scientist who helped develop Lipitor, the best-selling drug in the pharmaceutical industry’s history. Roger and his business partners sold their company, Esperion, in 2004, to Pfizer, for very substantial sums of money. The Newtons have become important philanthropists and proponents for many medical advancements, and they are also actively engaged in fostering greater appreciation for functional nutrition in academic and health care settings. Of particular relevance to this feature story, Coco has also been an important figure in the movement to change nutritional licensing standards in Michigan, and elsewhere.
Kirsten Mowrey, a licensed massage therapist, Trager® practitioner, and trauma healing therapist, interviewed Coco on several occasions for this piece. Kirsten contributed a CWJ interview in the last issue (Issue #59) on how the University of Michigan is training medical doctors to have a deeper understanding of complementary and alternative medicine
***
I first met Coco Newton over a decade ago. Back then she was raising a family, adapting to being a local celebrity (her husband, Roger, was part of the Lipitor team at Pfizer), and creating a nutritional practice focused on individual needs. Over that decade, diet, food, and food systems have been evolving in culture and healthcare.
I interviewed Coco, who is a registered dietitian and certified clinical nutritionist, on a fall day at her office in the Michigan Science Innovation Center in Plymouth. Her large office windows allow in a great deal of natural light and the room is painted a warm yellow. It has space for supplements, books, and a table for consultations. Coco herself was still the petite, vibrant woman who used gestures to emphasize her speech. When I arrived, she was just completing a conference call with the Michigan Nutrition Association, an advocacy group she co-founded to address legislative efforts on the state level. What follows is a wide-ranging discussion of nutrition, diets, professional passions, and personal journeys.
Kirsten Mowrey: What do you love about being a nutritionist?
Coco Newton: I love when someone who is really ill, really sad, and feeling hopeless comes and has been to doctors, usually several different doctors and specialists, and are kind of on their last legs, and I love it when they get better. Their complaint is gone! Watching people transform, helping people.
On the other hand, I really enjoy [that] each patient is this full mystery. You start from scratch; you don’t have a road map. I develop the road map to help them. The diagnosis is just a superficial descriptor; it’s the underlying processes that create this thing that we look at as a diagnosis, as a disease. One great book, Disease Delusion by Jeff Bland, [describes that] disease is just a name we give something; we are all about treating the disease, the name.
Someone will say: “What do you do for IBS or such and such diagnosis?” People must think I have a little file folder and I pull out what I do. But no, everything starts from scratch. I love the mystery, the challenge. It’s like being an investigator of the body and I’m allowed to go in and look for clues, looks for signs and symptoms, look at labs, look at the environment, hormones and exposures to find out how that’s affecting their metabolism and how that can interface with their mood, their energy, their guts. It’s all the factors.
Kirsten Mowrey: Do you feel nutrition is well understood?
Coco Newton: Getting better. Even though it might seem like more info equals more confusion. [What I] really notice about the public in the last ten years, across income, ethnicity, and age, is: I don’t want to have toxic food. I think there are more and more people concerned about nutrition. I don’t think it’s just a left-wing hypochondriacal group. They are also willing not to put all of their trust in one person, like a physician. They are getting frustrated with doctors.
I think the Internet has been fabulous for opening up ways for people to search and ask questions about their conditions in privacy. I get people who know nothing about nutrition but have read this book or that book and know there is something more. I got a call from Scotland because I was recommended in a book. This is what I mean about empowered patients: calling from Scotland!
I got a call from Minnesota. A hunter, he was like a lumberjack, he was suffering with gut stuff for years. He was like 70, and he got his doctor to do the tests and he responded really quickly. That doesn’t always happen, some take months and months and months, I never know what’s going to happen, you know. And I tell patients, if we happen to land on it quickly, then good. But you won’t see me beyond when you need to; my goal is to get you out of here really quickly.
So when you have people calling like that, who have never done this before, and they are really desperate, this is the modern patient, this is the person who is going to seek out their own healthcare. They are calling the shots on who’s managing it. Would you take your car back to a mechanic where it keeps breaking down? Wouldn’t you get a second opinion? Historically, we have had a certain loyalty to our physicians; we keep going back to the same person even if it doesn’t get better. We now hire physicians, we are not just a patient of an office; we are hiring them to do their job. That’s what I tell my patients [their] first day here. They are hiring me.
Kirsten Mowrey: What is a typical client visit like?
Coco Newton: Someone calls my office and before I even see them, we’ve done a lot of work. I have a 20-page form that goes into everything: gut, dental, environmental, family history, your own history, how you are eating and food records and food habits, three years prior of labs and central. This is so important: tell me your story. I get all this technical information. I know all the meds. If they are a woman, I know what is going on with their menstrual cycle. I know the doctors they are seeing. I want to know your story. I can look at everything, but you tell me what is your story. They are clues for me.
I see my work as a detective. Describe what was the last time you felt well. They’ll leave out things in a questionnaire like “my brother was killed in an accident and now I can’t eat this food” or “I had this virus and I was sick for three months and I got over it, but I’ve never been the same.” People often don’t think about what it all means. When people start telling their story, you get much more out of that than just filling out a questionnaire.
KM: First session, from intake form and face-to-face, then ordering tests?
CN: I like to base my recommendations on data. I do want a complete metabolic panel, a CBC (complete blood count), inflammatory markers, vitamin D, B12, but, in addition, I might need to test this person for adrenal or that person for iodine and genomics. Get all of my thoughts about why you are here and what your goals are; what needs to be done with food, supplements; what labs I need to fill in blanks; what needs to be written to the doctor; and environmental. Those are some of the big categories. It’s like a big algorithm. What questions do I still need answered? Is this a person I can do three changes with or one with all ten changes?
“The future of healthcare is going to be determined by the individual more than any single healthcare professional or institution. ”
One woman with MS, infertility, thyroid disease, depression, she was taking in a lot of aspartame (NutraSweet). I had her [stop aspartame] — do that one thing, I didn’t change anything else — and she went through a classic detox. Her whole body stunk for two months, her sweat, every orifice. She went through so much detox from aspartame. Her symptoms of MS disappeared. So what did she really have? She had aspartame toxicity. No one had ever asked her about her diet.
KM: What are genomics?
CN: When you are looking at genetic markers, looking at how different enzymes are working in the body, [it] helps design a personalized nutrition plan. Your genetics is not your destiny. It’s your environment. Epigenetics is more important than genetics. Epigenetics is [how] everything around happens around you that influences your expression and suppression of your genetic tendencies. So, for example, you could have a disease like diabetes that runs in your family, but let’s say you watch your weight, eat the right food, avoid toxins, get exercise, so those genes don’t get turned on. You may not express that diabetic tendency.
KM: Your way of addressing those epigenetics is through what you are putting in your mouth.
CN: And I link it to spirit and emotion. So, if you look at the Cheetos you bought and the organic carrots, you have kind of confusion of communication. In the beginning, I ask people to look at [what they are eating], because you never want to come with judgment. You don’t want to get into that bad and good, on and off the diet. I’m helping people fine tune their health through choices. The diet mentality has judgment associated with it, [a] black and white way of thinking.
Diet comes from Greek (diaita), which means way of life. Bringing people back to caring for themselves through planning around their diet, which they’ve externalized — they’ve externalized to fast food, to vending machines, to “we all happened to go to this restaurant so that’s what I ate.” No, you have choice. So it’s very empowering. The emotional part is people start thinking about what makes them feel nurtured and what makes them feel toxic. Once you start nurturing yourself with food, I ask them to look at their whole environment: Where else are you not making choices that are not nurturing — TV, books, people — not nutritious?
KM: Thich Nhat Hanh talks about this. What are you taking in through all your senses?
CN: When you start to respect your body, when you see the Cheetos as a form of disrespect, not just a bad food, but a form of inflammation, a form of toxicity, then it’s not like, “Oh, I’m eating the healthy foods vs. unhealthy foods.” You see these foods as carrying a form of energy with them that is really negative. So I really help people connect what they are doing in their world and food and wake up. And it’s interesting to watch that process. People kinda get: “Oh, if I can make choices around these things, I can make choices in areas of my life I was choosing not to make choices. I really could walk, I really could meditate for ten minutes, I can move, I don’t have to be so patterned in an old pattern.”
KM: Makes sense, once you’ve shifted the habit energy, as Hanh calls it, the whole pattern reforms.
CN: He is one of my favorites, and I have a saying of his on mindfulness and food in my folders that I give my clients the very first time. First, it is about respecting that [food] comes from someone who has grown it; it goes through many hands before it comes to you. That work and effort, and being mindful about your food when you shop, cook, eat — all of that is a gift. We’ve gone so far in the opposite direction in this country, you are almost rewarded for how little time you spend in the kitchen. Mealtime and eating has become a thing of the past, and I do meet people who have never had meals at home, who have never cooked. It’s easy to eat and not be in the kitchen. It’s a real cultural shift to bring people back to the eating world. That’s a part of this too, even though it’s very scientific, it’s very medically oriented. It’s also about creating the whole eater. I think people are really wanting that deep down.
KM: What is the difference between a nutritionist and a dietitian? Is it location?
CN: That’s the best question! So a registered dietitian is a four-year undergraduate degree and an internship, mostly in hospitals, and they have to pass an exam. Every dietitian is a nutritionist, but not every nutritionist is a dietitian. Nutritionist is someone studying nutrition beyond the institutional acute care model. The dietetics model does not teach personal biochemical individuality, it is not personalized like that, it is far more disease oriented.
The nutrition training I received goes into a functional medicine approach, based first on biochemical individuality, not just looking at the absence of disease but for optimal function. It goes deep into lab evaluation and personalized care.
Most of these certifications, some are through universities and some are not. There are private institutions that have sponsored these certifications... Forward thinking and mobilizing in education in nutrition is not happening at the university level, it’s happening at these private institutions that are doing this. What the public needs is access to nutrition. We have, given our population in Michigan, if we only allowed dietitians to serve, we’d be serving .001 percent of the population. There’re very few dietitians in private practice as opposed to institutions.
KM: It strikes me that what you are talking about (certifications) parallels what is happening with food itself: patenting of seeds, and saying this seed will always go this way.
CN: Just as there’s no one authority on seeds, there’s no authority on the future of food. It is a right. Same with where you get your information. It’s unrealistic to think that people won’t go online, or read books, or talk to others. People are drivers of their health now, and this is a huge shift in healthcare. It’s uncomfortable for people, but it’s also liberating. The future of healthcare is going to be determined by the individual more than any single healthcare professional or institution.
KM: That’s a profound change.
CN: It’s our responsibility to educate ourselves. Like guidelines for choosing a nutritionist: I would want to know the person’s educational background, because if I’m going to assume there’s no one place to go for a nutritionist, what are my criteria? What did you study? Where did you go? How many years have you been practicing? What are the areas where you are really confident? What are areas you don’t get into? What kind of relationships do you have in the community? Do you cross refer? Do you work with anybody else? Do you evaluate lab reports and in-depth ones? Do you look at genetics? How do you charge? Do you charge for face-to-face? Do you charge for non-intervention? How do you educate about food? How much help will I get? What’s your follow up?
You really want to get a sense of what to expect. You want to develop a sense of trust. You want to know as a client what you are getting into. I am tenacious on behalf of a patient. If a patient needs certain labs for me to do a proper assessment, I will write a letter to the doctor and ask the patient to lobby for themselves to get those labs.
“I grew up in the 60’s. I was a flower child. I hung out in the Haight-Ashbury, that was a big part of my childhood...”
KM: Will physicians order labs in response to your letter?
CN: It’s all about empowering the patient to be their driver, and if the doctor refuses, many patients will quit their doctor and find a new one. Patients who come here are often on their last legs. I’m seeing people coming here who are deeply sick and going down. It’s amazing the way people will get behind their own lives when they need to. It’s an amazing satisfaction.
KM: How does nutrition fit in the allopathic model currently?
CN: Not fitting really well. Twenty percent of programs offer something in medical school. [Physicians are] not tested for it on their boards. [It’s] not something they have to be competent in, so unless they have an interest, they don’t pursue.
KM: How would you like to see that change?
CN: Oh, big time. That’s a lot of what I am involved in. People aren’t being served in their doctors’ offices. Well, first, it has to include applied nutrition in medical school. Not just recognizing deficiency: Why is this person tired but they don’t have a disease? Why is this person’s skin acting this way when they don’t have a disease? It’s never addressing the underlying issues, and that’s something functional medicine does: it goes to the underlying upstream issues. It could be one upstream issue that is creating all these symptoms.
KM: Can you give a real world example of that?
CN: Real easy one is gluten. It can cause gut problems, skin problems, headaches, joint pain, mood disorders, so you’d be off to all the specialists and it has something to do with your diet. And you many not even know to look there. Another possibility is dysbiosis, like a yeast overgrowth, or leaky gut, and once you have leaky gut, you get immune responses all over the body.
KM: Things that are big in nutrition right now — gluten free, paleo, organic, low fat — what parts of that [are helpful]?
CN: There is no one diet that is good for everybody. There are elements of many of the diets that are good for everybody, but that’s where you have to work with the individual because sometimes the diets come across as a religion. If you don’t do this, you are not going to be healthy. There’s a lot of fear-base in diets. I think it circles to some fear of, If I don’t do this what’s going to happen to me? I have patients who cannot tolerate any carbohydrates. If they put a cracker in their mouth they will be sick; it doesn’t matter if it’s gluten-free or not. They have different metabolic issues than someone else who can handle a grain. There are people that do much better on higher healthy fat diets. And paleo is not paleo is not paleo, so what is really paleo?
KM: [laughs]
CN: It is an idea and I don’t want to get into the debate about the different diets. I’m not there. Can’t you just all get a grip and look at what is best for the individual and not be ideologically attached to the point? Sometimes it feels like zealots!
I will borrow this from someone else: the “don’t eat crap” diet. What is crap? Processed, GMO, too much sugar, all the junk out there that we all know is junk.
KM: Our diets are also very regional and cultural — you are originally from California, correct?
CN: Yeah, I grew up in San Francisco. My parents divorced when I was 15. I grew up in the 60’s. I was a flower child. I hung out in the Haight-Ashbury, that was a big part of my childhood; I could just get on the little municipal bus on my corner and get straight there.
KM: How do you think that influenced you? How did you incorporate that experience?
CN: A lot, because I participated in all the peace marches. My high school was an open forum high school; the Hare Krishnas would come through, the Jesus Freaks would come through, Chinese gang wars, we had everything going on. I would cut classes to attend peace marches wherever they were in the city. I really developed my own identity. Even though I was following crowds around, I developed searching for my identity.
KM: After that did you go right to college?
CN: I applied to be a foreign exchange student; [Rotary] chose for me to go to India. That was before college. That was 1972. I was in Ahmedabad. I was near what back then was West Pakistan. I was on the outskirts of a city, so it was like a village.
KM: Was your mom in healthcare? Had you had any exposure to Western medicine?
CN: No, she wasn’t. I was fascinated; I didn’t know anything of India before I went. I lived and traveled with a doctor and his wife, traveled by Jeep to a village. He would go every other week to dung huts that were his surgery. I would be with him all day long and he would translate the cases into English for me. I would stand as close to him as I am to you [2–3 feet] and watch the surgery, [a] laparotomy (abdominal surgery). I watched him do a hysterectomy and [I was] swatting the flies away. That was an experience; it opened my eyes so much. I came back, I had malnutrition, I was anemic, I had worms this big in me [gestures with hands 4 inches apart]. I looked anorexic, I was pale. [The trip] grew things I couldn’t intellectually capture. Open, curious, adventuresome.
KM: Then you returned and went to college. That was where you got your first degree as a dietitian, yes?
CN: I figured out I wanted to do something where I helped people and I wanted to have something to do with science. I liked the field of nutrition and the only way to get into it was through dietetics, but I was a fish out of water in dietetics from the very get go. The head of the department — I wanted to get an internship so I could become a registered dietitian — she told me, “I won’t write you a letter of recommendation. I don’t want you in the field.”
KM: Wow! I wonder what she would say now.
CN: I stayed and graduated. But I couldn’t get an internship because you had to have a letter from the head of your department, so I went to graduate school, in Minnesota, and got my master’s in public health and nutrition. So from California, UC Davis, to Minnesota. The rules were if you had your master’s degree in nutrition, you could get an internship. You didn’t need that letter of recommendation.
KM: So you went to school for two years to get around this requirement. I was going to ask where Roger came in during all this?
CN: We met at UC Davis, 1976. He was getting his Ph.D. in nutrition. He oversaw the labs for all the students in dietetics and nutrition. He was behind the scenes. I didn’t have a clue he existed. It was the end of the semester, every department had their own potlucks, and I was going to go to the animal physiology potluck because I thought it’d be more guys, less women there, [laughing] because dietetics was purely female and I knew them all! So then this guy comes into our lab, being Roger, “Could I please have a show of hands of who is coming to our potluck?” I ended up going because I thought he might be there. When I got there we started talking a little bit, and he says, “So, what did you write your term paper on?” I rolled out the title of it: “The Use of Intra-Lipid in Total Parenteral Nutrition.” He looks at me and says, “You wrote that paper?”
What hospitals had was only protein and fats in their total parenteral nutrition, which is the same as intravenous nutrition (feeding via the subclavian vein and bypassing the G.I. tract). Lipids (fats) were being used in Scandinavian countries, but hadn’t come to the U.S. yet, so I wrote a paper on it in parenteral nutrition, which was cutting edge. My husband is a lipid specialist. The head of the nutrition department had handed him my paper and said, “You’ve got to read this paper. It’s right up your alley.” So he read the paper, but he didn’t know who I was. A year later, lipid feeding came to the U.S.
KM: You were ahead of the curve! What happened after meeting Roger?
CN: He asked me out a week later and we’ve been together ever since. He got his master’s in nutrition and his Ph.D. in lipid biochemistry. It came time for him to get a job and he got offered a job at Procter & Gamble. I was in grad school working on my master’s and he said, “I’ve been offered a job at P&G.” This was the time of the Rely Tampon and toxic shock syndrome was all over the news, and I said, “I would have to be in love with you enough to marry you to go someplace like that [P&G].” I said it sort of tongue-in-cheek, but I really didn’t want to go to Cincinnati in the midst of this. He goes, “Oh, you want to marry me!” and that’s how we got engaged, over the phone and tampons! [laughs]
KM: That’s great!
CN: [After my master’s] I did my internship in San Diego at UC San Diego. I was working in a hospital environment. From there, I did the WIC program for the County of San Diego and that was awesome. It was so fascinating. San Diego County had such a diversity of different cultures. You went someplace and it was Hmong, and another place and it was all Native Americans, or blacks or Hispanics or some places mixed. It really gave me an appreciation for interviewing people and learning about all the different food habits and beliefs. I was fascinated with [the Hmong,] how the breakfast, lunch, dinner was all variations of the same theme. Vegetables, lots of vegetables, and onion and garlics, always rice, then either fish, chicken, or beef. It was repetitive but diverse at the same time.
KM: When you’d finished with the WIC program, what next?
CN: Well, I did want to work in a hospital, and I got into a small community hospital near the border of Mexico, like 120 beds. Tiny. The beauty of working in a place like that is there are not layers of bureaucracy, so if you have an idea, you can take it to the head of your department and it goes right to the administrator. As a community hospital, I had talks with the community and educational programs.
And I had this fascinating interest in patients in hospitals that were basically starving to death. It was people who, say, have had different surgeries, and have to have nothing by mouth for a period of time, or they can only have clear liquids and they gradually are starving and no one really notices because you are so busy dealing with all the medical procedures. Then malnutrition sets in and it causes its own cascade of problems, infections, and poor immune system and all that. I got into the field of critical care nutrition, like I.C.U., or medical patients so ill they are malnourished. I really became interested in that and learning how to develop intravenous feedings and tube feedings.
Roger was doing his post doctorate fellowship as I was doing the community hospital and the fellowship was going to end, so he accepted a job at Parke-Davis. We thought it was a five-year plan; we’d be back in California again. That was 1981. It was much more.
KM: You came to Michigan and got a job at a hospital? Were you and Roger cross pollinating professionally?
CN: Not then. We did teach classes on nutritional biochemistry to dietitians on the side. We started this nutrition biochemistry update. We would get a room at St. Joe’s and he would talk about nutritional biochemistry and metabolism, which was fun. After that, he was in the pharmaceutical world, and for a while there I felt like we were on way opposite ends of a spectrum and there wasn’t much cross pollination. I was doing dietetics, but I was still really interested in finding those starving patients in the hospital, that was my mission. I had co-started a critical care nutrition support team when I was in San Diego and I did the same thing at St. Joe’s Hospital. There hadn’t been a team before I and the department of surgery, critical care nursing, and pharmacy [became one]. I was really interested in that. That wasn’t what I was hired for, but that’s what I ended up doing and they really liked it, the doctors really liked it. It was so interesting, because nutrition was so not appreciated by physicians back then, but there were a few who got it and we really bonded. Now the dietetics department didn’t get it at all.
KM: That would have been 1982, this was happening?
CN: 1982, and I ended up being let go by the dietetics department for insubordination, in their mind. I told the doctors and the pharmacy and the nursing department and they were aghast. They all wrote these really, really strong letters to the hospital administrator, human resources, and my department about the value of my work. There was no real insubordination, back then departments could get away with a lot without documentation, they were going to take all my benefits away, my pregnancy benefits.
“It’s really not about whether you have celiac or not, it’s a spectrum. ”
KM: You were pregnant with your first child?
CN: Yep, my first. [Dietetics] just wanted to get rid of me because I was doing all this work that was really valuable to these patients that the dietetics department said, “We don’t deal with those patients because they are not eating.” I’m saying: “We deal with them because they have malnutrition. Aren’t we nutritionists?” “No, we’re dietitians.” That’s where I really felt the difference in those terms. “We deal with people who are on diets.” Well, who’s going to deal with the people who are falling apart because they are not getting their nutrition? And many times it wouldn’t be ordered until it was too late.
KM: What happened?
CN: They changed the leadership. My boss was demoted. They brought in a really progressive woman and I got asked to come back.
KM: Did you go back?
CN: I didn’t go back. I think it’s great they changed the chain of command there. I just didn’t want to go back. I was in a different space. I had just given birth to my oldest son and was home for less than a week and I get this random phone call from a woman I had met a couple times. She had a private practice out at Ann Arbor Family Practice, she was leaving town and wanted me to take it over. I was the only person she could think of. I went there and everything had to start from scratch, just like that. I was really a typical dietitian at that point; in the hospital, I was only interested in working with high-risk people, not just the “show someone how to eat a low fat diet.” When I transitioned to people who not only weren’t in a hospital, who just ate food and came in to be [placed] on a diet, I really didn’t know what I was doing. So I found materials and developed my own style. I then became very disenchanted. I had like a mid-career, mid-life crisis. I felt that I wasn’t really helping people…. I didn’t feel like I was being of service to the level of purpose that I felt that I had. I felt like I was held back.
KM: How soon did this happen, was this like three months, a year?
CN: No, no I did a lot of things, I had two more children. I started the practice in 1983, and I started going into the identity crisis in my field in probably 1990. I just felt like it wasn’t intellectually challenging. It’s so formulaic; dietetics is so formulaic. I felt like I did more individual biochemistry in the hospital patients who were critically ill. I felt like I was very superficial in this [private practice]. It was all about seeing if someone gained weight, lost weight, cholesterol up or down, sugar up or down. You didn’t get into pain or fatigue or medical issues — that was left for the doctors. Everything you did was from a doctor’s order. I was in a physician’s office and they sent me people who wanted to be on diets.
KM: So what did you do?
CN: I almost totally quit the field. I was looking into Ayurvedic medicine, naturopathic, homeopathy, herbal medicine. Then I started meeting people, naturopaths and others who called themselves nutritionists. They had all this enthusiasm and they were actually practicing using nutrition in their practices, using information that I had never heard. Where were they getting all this information? Why is theirs so much more sophisticated than what I’m doing? Talk about low self-esteem! I was excited for them, but I didn’t even want to tell them I was in the field, I didn’t know what to say. I just felt so inadequate. With that, I knew I was either going to find a way to get into nutrition somehow that felt right to me and totally change my practice or I was going to leave altogether.
KM: At this point, you and Roger hadn’t been working together.
CN: No, Lipitor was approved in 1996, so he was in process. This was about a 10-year period, in 1994 it really crescendo-ed. I really, really felt it, but it was growing before that. In 2000, I heard Jeff Bland speak — that was a seminal moment for me, May 2000. It was a six-hour seminar he gave and I was at the edge of my seat the whole time, taking notes the whole time, every word, it was like, OMG, yeah, this is what nutrition is about.
In 2001, I went out to the Institute for Functional Medicine. I was really nervous to go out there. I was so self-conscious about being so behind in nutrition. The people who are there are doctors, dentists, but you can go if you are a nutritionist. I loved it and everybody was an equal, because everyone came there to learn, and it was like taking a sip of water from a fire hydrant, so much inspiration. I came back, I was in my office, [asking] how do I implement all this? Just a step at a time, but I never turned back. I’d never left private practice. I’d slowed it down, so I began studying and taking all these courses and building my clinical skills. I became a certified clinical nutritionist in 2003.
KM: How did your training affect the way your kids grew up, the food they were given?
CN: I was one of the first people to go into Whole Foods when they opened here and my kids are like, “Nobody else goes here!” And I was like, “There’s a bar, you can go sit at the bar!” All the enticement! That was back when they didn’t understand why I never served processed food. I didn’t eat like dietitians, oh gosh no! I remember when I first came to Michigan, at the University dietitians’ weekly meetings — remember, I came from California, the land of granola, fruits, and flakes. I came and they had all these donuts and sweet rolls and coffee and that was all they served at these meetings and I was like, “What is going on here!?” I just couldn’t get over it! So I was already different.
KM: Did you make your kids lunches?
CN: Oh I did! They all felt that there is nothing to eat at our house. “I wanna go to so and so’s house because at least their mom has things you can take out of the cabinet and peel off and eat!” Like the Lunchables and that. “Why do we just have food, like real food?” I would make a homemade macaroni and cheese back then. “We want the ones that you squirt out of the bag!” They didn’t get it then.
KM: Do they get it now? Did they reconcile themselves to how you cooked?
CN: Oh yeah. All of them eat really, really well. I have two sons and a daughter. They are all gluten free. Two of them really need to be and the other one plays it for a while and then he has to go gluten free. They reconciled themselves when their friends came over and said, “Dude, you’re really lucky. Yeah, I like this food, what are you complaining about?” Their friends really loved it and it got our kids to look at me through someone else’s lenses. I had peer approval for the most part. Even little things like fruit and veggies, they didn’t want, they wanted cookies. My oldest is 31 now, then a 29-year-old son, and daughter, 26. When you talk about our kids and diet, our oldest son has really, really bad responses to gluten. He’s never been tested for celiac. Genetically it doesn’t show he has celiac but he definitely has gluten intolerance.
KM: How did you find out?
CN: Well, I didn’t know what it was. He had aches. After eating, he felt terrible, sores in his mouth, boils, [felt] more wound up. I found out when I started functional medicine. Early 2000’s, I converted my family. It was gradual. Him first, because his gut was giving him a lot of problems, it was urgent. My second son doesn’t have it as bad, his gut doesn’t feel good. And then my third, she would feel it in her brain, big brain fog, like someone had slipped her a drug. I must have a gluten response someplace in my body, but I don’t feel it. I just don’t have it in my house, for my family.
KM: In November, there was a piece in The New Yorker about the increasing number of non-celiacs eating gluten free even though they are not diagnosed or testing as celiac. There is no testing evidence to support gluten sensitivity. What is your opinion?
CN: Testing is a very important part of diagnosis. Unfortunately our testing is not sensitive or specific enough to give us a good diagnosis. Ideally, everybody would like to know absolutely yes or absolutely no, what is my issue with gluten? Gluten is a spectrum; celiac is the far end result of damage. Celiac disease is something you can pick up on a biopsy most of the time, but not always. You can have non-celiac gluten enteropathy, a lot of damage in your gut, even without celiac disease and it can cause the same manifestations not only in the gut but the whole body. It’s really not about whether you have celiac or not, it’s a spectrum and that’s where I think a lot of media has looked at criticizing the popular notion that there’s anything beneficial to going gluten free unless you have documented celiac disease. There are so many people who are non-celiac who are very, very sensitive to gluten to the point that it makes them ill.
KM: The article talks about vital wheat gluten, a common additive in commercial bakeries. It is described as brick-like. I have heard suggestions that additives like this are the trouble — that bread is a long, slow process, and as a result of that process, it’s more digestible. I have read of bakers that do a two-day rise, and, as a result, people who have a gluten allergy can eat the bread. There is a component of time.
CN: I have heard that from dough to bag is a really accelerated process, hours. It’s not even bread, as we know bread, which you knead and rise and punch down. Also that there is less diversity of grains and ancient grains which aren’t being used and there’s the processing. Although we’ve had processed bread for a long time, it’s a question of how deeply it’s been processed.
I come from a baking family — this is so embarrassing, but it’s kind of funny! My family was the white sliced bread company for the West Coast. My grandfather in the 1930’s, Langendorf Bread. I came from sliced white bread: undo the karmic fallout! The way I look at it is, when people say they go off gluten and they feel a whole lot better, I don’t even care if they have a blood test, they don’t care. This debate over when is it real, when is it not: it’s real when it happens to you and it works to be off gluten. It depends on where you are in that spectrum and what other ways your system has been assaulted through your diet. It’s your immune system that’s reacting, and it underlies many autoimmune diseases. I had a 62-year-old man in here and when he went off gluten, it had a stream of effects through his body. He’s not diagnosed with celiac, he doesn’t care. He just knows he lost all his belly fat, he is able to concentrate, and he has much better exercise tolerance. It affects his mood.
KM: With food allergies, since your cases are complex, it’s just part of the package?
CN: Every practitioner is really different about this. First, what I like to do is go with an elimination diet in the beginning, or maybe just eliminate gluten. I try to gauge people’s readiness for how much and I don’t like to overwhelm people. But if you do an elimination diet, you are getting rid of the major offenders — dietary — that doesn’t mean you might not be allergic to other things, but at least ruling those out. Also, what came first, the allergy or the food? If your system is immunologically challenged, if your gut is leaky or inflamed, or your pancreas doesn’t put out digestive enzymes, there can be an immune up-regulation to lots of foods that come in, and that’s because your immune system is so inflamed, is on such high alert, that every food can be an allergy. When you heal the gut, calm down the inflammation through diet, through herbs, through supplements, you may no longer be allergic to foods you were allergic to. There will be some that will remain. That’s what you have to sift though as a nutritionist.
KM: The major offenders are?
CN: Gluten, dairy, eggs, shellfish, alcohol, caffeine, soy, corn, peanuts, sugar. You know, that doesn’t mean you can’t be allergic to a strawberry. With a strawberry though, you eat it and get an immediate effect; with the others, you get delayed effect [from major offenders]. So, we’re not talking about immediate immune reactions. You have an IgE, Immunoglobulin E, response to that strawberry, but many people have delayed response, that’s an IgG, Immunoglobulin G, response and those manifest, that can be 12, 24, 48 hours later. It can manifest differently: headaches, hives, G.I., fatigue. Brain fog is another. So is pain, joint pain. Those aren’t immediate hypersensitivities.
KM: How do you educate people about food to not simply think, I go to the grocery and there is food, but the whole cycle?
CN: I do it in a non-fear-based way. If it’s done in a top down, fear-based, “You gotta do it to avoid A, B, & C,” that’s not how I talk. I really talk about being connected to our food supply, being able to appreciate the wholesomeness of a food, which is very different from good and bad. Also, that food will support you at a cellular level, into the deepest part of the body, because we often think food goes through the gut and out. I want them to think of it as something that is bringing goodness into their life, good mental and physical feeling, healing. I try to bring it into real life, I say, “What is a good friend to you?” A good friend is trustworthy, pretty transparent, makes me feel good, is there when I need them. There is a relationship.
KM: Your clientele is already self selecting then?
CN: Yes, and they are paying out of their pocket. This is a commitment. It’s a personal commitment to themselves. Some people are on a really, really tight budget. They’ve had to maybe borrow money to do this. Some people are OK to have this in their budget, and others, it doesn’t matter. But I can tell you I definitely don’t cater to a wealthy clientele, not out here. [If my client is a kid,] most parents, by the time they come here, they are pretty willing. Also, food is hip now. When I was practicing just dietetics, food wasn’t hip at all. Food has caché now. It has a lot of swag, so it’s popular. It makes it easier to be a nutritionist. You know, this person comes in and they really have to eat truthfully with themselves; it can spark some real transformations.
KM: Where do most of your people come from? How many clients a week?
CN: This office is on the border of Plymouth and Ann Arbor. I would say I get a lot of people from Plymouth, Novi, Northville, Ann Arbor, the whole area. I also get people from Chicago, Toronto, Ohio -- who drive. I also see patients international, via phone. I’ve been seeing patients Tuesday, Wednesday, and Thursday. About ten a week.
KM: With the rise of technology, many people are using apps to track their diet. What do you think of these, about tracking what you are eating?
CN: I’m not personally into it. For patients who have their apps and bring it in, I don’t discourage them. I feel eating is more than tracking carbs, fats, proteins, and that’s usually what those apps are being used for, behavior modification. I’m not against them, but I never talk about it with people.
KM: What don’t you like about being a nutritionist?
CN: There is a passing feeling. I can feel so sad for a patient, but I would call that a challenge. The admin part is huge, having good backup and organization. Being HIPPA compliant is huge and staying on top of all those rules is huge. Paperwork, lots of paperwork.
“[I talk to clients about how] food will support you at a cellular level, into the deepest part of the body, because we often think food goes through the gut and out.”
KM: What else would you like to tell us? I know you want to spend more time on ALS, which takes you back to your roots, with feeding tubes.
CN: I want to do writing. I want to work with my patient, Craig Oster, who is amazing. He is someone I’ve been working with for a few years and he is a 20-year survivor [of ALS]. One of the things we want to do is influence the ALS Association, which currently has horrible nutritional guidelines. I mean, not based on science, actual guidelines that will make you for sure sicker. It’s full of very processed foods: put all the Hershey’s syrup on it because all you really have worry about is calories. We want to have a talk with the ALS Association. We’re involved in a book and a film (www.healingals.com) on patients around the country, who, in different ways, cleaned up their diets and detoxified, brought in supplements and mind body techniques who have reversed their ALS.
I worked with one ex-NFL player who had ALS. He looked like he was blown up like a balloon, he had diabetes, was insulin dependent, and he had ALS and gut problems. He was tube feeding, like Ensure. All I did was find a whole foods tube feeding, genuine tube feeding, switched him from processed to whole foods, and he no longer has diabetes, he no longer takes insulin, his gut is good, and his face looks like a face. He may have not reversed his ALS per se, but his quality of life has improved. But if you were to look in a dietetics textbook, they are going to say that all you need to pay attention to are calories, and they [patients] are going to live 2–5 years. It’s a death sentence, ALS is a death sentence. But what we’ve learned from my patients is you detoxify, you bring in nutrients and foods that support the nervous system that are anti-inflammatory and allergenic, you can do a heck of a lot. This is a real example.
I’m very much in service, because we are going to go to bat with the ALS Association, myself and some other neurologists helping to get the guidelines changed for ALS. They are back in the 70’s. Let me show you one thing — it’s like a time warp — now if they’ve changed it, because we’ve been talking to the media [goes to computer and looks]: “Maintaining good nutrition with ALS — document from 1999, last time updated!” Everything in here is processed food. Everything! Canned fruit, ready to eat cereal, instant breakfast milk, canned soup, dry milk powder, “foods high in fat and sugar are good sources of calories,” margarine! “Add syrup!”
KM: This must make you shudder!
CN: This is what we are up against: “add commercial thickening powders to soups,” “prepare food with Jell-O.” You could say this about any disease, especially the neurological diseases: Parkinson’s, Alzheimer’s, MS. I am really ready to focus on this and am constantly doing research.
KM: Has your work coincided again with Roger’s, as you get into individual biochemistry?
CN: Roger and I started coming together again when I started getting into functional medicine. It was getting into nutritional biochemistry again. Straight up dietetics doesn’t really get very deep, but when you get into functional medicine you are really getting into individual biochemistry.
…We are both advocates for more people being educated in functional medicine, especially dietitians, as they can be the carrier molecules of this information. Right now you look at most institutions, which is where dietitians are, [and] we need functional medicine to be the standard of care, not something you have to pay extra for, outside of the system. A big part of our work together has been supporting programs and helping to organize programs to bring a change in dietetics education.
KM: Is this like seminars you did at St. Joe’s?
CN: In a bigger way, we are trying to get changes across the country. We’ve been working with KU (University of Kansas), because they have a really strong integrative medicine program… What we did is we organized and helped support a connection and a working together of the Integrative Medicine program with the Department of Dietetics to bring dietetic interns and students into the world of integrative and functional medicine. Because they don’t get exposed.
KM: Are you teaching those younger nutritionists?
CN: I have been involved in teaching, but I’m not teaching at KU. But I have been involved in the curriculum planning and in setting a standard. Because this is how I look at it: everyone should be looked at as an individual. Dietitians are not taught individualized nutrition, it’s very cookbook: If you have diabetes, you give the diabetes diet. And it’s still taught that way. What we want to inspire and get done is a ground swelling, from the ground up, a demand by departments and dietitians to have a better education that includes this level of training.
I’ve also worked through the Institute of Functional Medicine with this and we have identified key dietitians out there in the country who are in influential positions, like authors of textbooks, researchers, clinicians…
I do a lot of career counseling, nothing official, but people call and ask, “What should I do with my career? How do I get where you are?” We have so many dietitians in this country, how much healthier we could be if we could train those dietitians (1,500–2,000 in Michigan) to do the work their nutrition calling should be about. I want to see more people doing the work. I want to be able to refer to more colleagues. There need to be more of us doing this.
KM: Anything else you want to say?
CN: I feel like, for people, don’t accept the limitations of what you might be told diagnosis-wise and prognosis-wise. I’ve had people come and they are so afraid of what they have been told, diagnosis-wise: “I’m sorry there is nothing we can do for you.” And never give up. Craig is an example of never give up. When you work for someone, you are working to get them further. So you have to find someone who is really going to work for you. You are hiring me. I’m not just this person to just give you a diet and supplements. [I want] For people to really be consumers of health care and not to give up. Do your homework, ask all the questions you need to. You need to trust the person and not be afraid to ask a lot of questions.
Coco Newton is a registered dietitian and certified clinical nutritionist. Her office is located at 46701 Commerce Center Drive, Plymouth, Michigan 48170. For more information or to make an appointment, contact her at (734) 233-3075 or email her at coco@coconewton.com.




























To build your pelvic power, it is vital to de-stigmatize the pelvis and its functions. No one feels uncomfortable talking about their arm, leg, or stomach muscles. There are dozens of classes and machines at the gym for building flexibility and strength in these areas—yet none for your pelvic floor.