by Namita Sachdev, MD and Elizabeth Shadigian, MD
Managing any illness is challenging, and conventional medical care—the current “doctors at the top and patients at the bottom” status quo health care (SQHC)— provides diagnosis and treatment of acute life-threatening illnesses such as a heart attack, stroke, or pneumonia with mostly excellent results. Acute illnesses such as these require an immediate, short-term, reactive approach and generally resolve once appropriate treatment is completed.
In contrast, treatment of a chronic illness is most effective with an incremental, long-term, proactive approach to managing symptoms. However, SQHC has not yet evolved to treat chronic illness optimally. A chronic illness is life-long and has symptoms that come and go or are present continuously. In many cases, multiple chronic illnesses exist simultaneously.
When you have a chronic illness, a health care provider may not know the exact diagnosis and will tentatively use “a working diagnosis” while a full work-up is pursued. During this time you will still have to cope with symptoms and may not have a clear treatment strategy yet. You may feel like congratulations are in order when your chronic illness is first identified or diagnosed. It may have been many years of scattered symptoms and multiple health care visits to generalists and specialists. You may have had feelings of self-doubt and uncertainty about your symptoms until the reality of having a chronic, serious health condition is confirmed.
SQHC has divided health into two broad categories of body and mind and treats each category separately. All illness has physical and psychological components, and it is necessary to treat both the body and mind simultaneously, especially with chronic illness. When a chronic illness is finally diagnosed, physical symptoms can be overwhelming and difficult to manage. You may also have upsetting thoughts that recur in combination with feelings of fear, frustration, loss, or anger. The physical and psychological components always work together, and to treat only one will not produce long-lasting beneficial results.
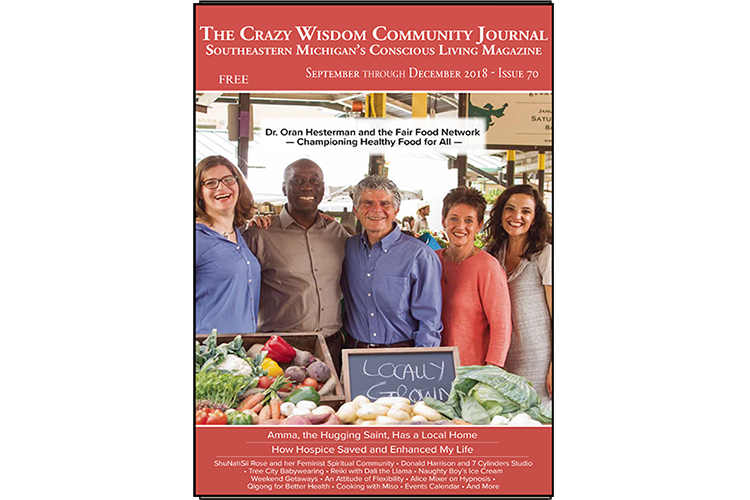
Read related article: Be Brilliant! How Hospice Saved and Enhanced My Life
Chronic illness is characterized by ongoing physical and psychological symptoms that worsen and improve over time. Patricia Fennell describes the four phases of chronic illness as crisis, stabilization, resolution, and integration, in her book The Chronic Illness Workbook. This four-phase model describes how you may experience chronic illness and how to identify which phase you are experiencing. Understanding the signs and symptoms of each phase can help you develop and implement management strategies—ways to cope with your illness.
For example, during the crisis phase, medical treatment can be complex. Partnering with your health care provider and building a team of health professionals can be a slow and frustrating process. Some of the strategies in this phase require ensuring your own secure physical space and learning to hang on through the changes and suffering which may occur. A chronic illness can create feelings of trauma, loss, and grief that are unique to each person. Acknowledging and recognizing these feelings can give you insight into what is happening to you and can help you better manage the crisis phase. Another important part of caring for yourself during this phase is to ask to see your health care provider more frequently based on your physical and psychological needs. You may want to have separate support from a counselor or psychotherapist as well.
Having a health care advocate at your visits during the crisis phase can also be helpful to assist you in gathering information, providing support, and advocating for yourself. You can get the best out of your health care experience by having another set of eyes and ears with you before, during, and after medical appointments. At WomanSafeHealth, the term “woman advocate” is used and applies to clients of any gender seeking care. A woman advocate differs from a health care advocate in at least three important ways. A woman advocate is aware of the: a) woman seeking health care’s particular herstory, b) power dynamics in all health care settings, and c) sexism and other oppressions women are up against seeking health care. A woman advocate can be a friend, family member, colleague, or trained professional.
Feeling empowered to ask for information about treatment options, risks of treatment, and the time frame for decisions will develop over time.
Since most of the care given to the person who has a chronic illness is given by herself or himself, the care given by you is essential, necessary “self-care.” You are also making multiple daily decisions to manage your illness. As you enter the stabilization phase you may look for others with a similar illness. You will have greater control of your symptoms, but you, your friends, and family may still have difficulty accepting that the illness is ongoing or chronic. Your symptoms will likely worsen some days and your physical capability may change from day to day. These fluctuations can lead to uncertainty and variations in mood. The goal in the stabilization phase is to develop an “observing” self; this will help you pay attention to what you do and how you do it. By tracking your symptoms to look for patterns, restructuring your activities based on your physical boundaries, and learning to understand your thinking patterns, you can learn to manage your symptoms over time. When you are empowered, involved, and feel competent in caring for your chronic illness, you have a tremendous positive impact on the outcome of your illness and your quality of life.
As you move toward the resolution phase you accept your illness as chronic, and as your “observing” self develops, you recognize the triggers that increase symptoms. You understand there is ambiguity in the course of chronic illness and have compassion for yourself. You begin to reflect on the change in yourself from your pre-illness self and develop insight into your losses. You are able to maintain a more stable and meaningful life. A linear progression through the four phases of chronic illness does not exist. Symptom flares come and go, and over time your ability to anticipate flares and head them off improves. In the integration phase you understand that recovery, stabilization, and relapse are part of the normal cycle of chronic illness. You develop a new “personal best,” engaging in joyful activities and integrating the chronic illness into your life. So, congratulations on your diagnosis and your ability to cope and thrive.
WomanSafeHealth is a safe, respectful, and compassionate practice in which each client defines and obtains empowering WomanCare and Gynecology health services. The guiding principles for WomanSafeHealth care providers are: I welcome you, I listen to you, I believe you, I protect your privacy, I am accountable to you, and I respect “no.” WomanSafeHealth’s Woman Advocacy Program is available to the community (womansafehealth/services/advocacy). For more information contact WomanSafeHealth at (734)-477-5100 or email info@womansafehealth.com.
Namita Sachdev, MD, FACP, FAAP is a board-certified internist with over 30 years’ experience caring for clients, especially those with chronic illness.
Elizabeth Shadigian, MD, FACOG is a board-certified obstetrician-gynecologist specializing in the health, safety, and wellbeing of women. She left academia as a Clinical Associate Professor to create WomanSafeHealth, a medical practice and new model of health care based on women’s empowerment.
Dr. Shadigian’s book, WomanSafeHealth: The Antidote to Status Quo Health Care was published in June, 2016 and is available at Crazy Wisdom Bookstore.
Related Articles:








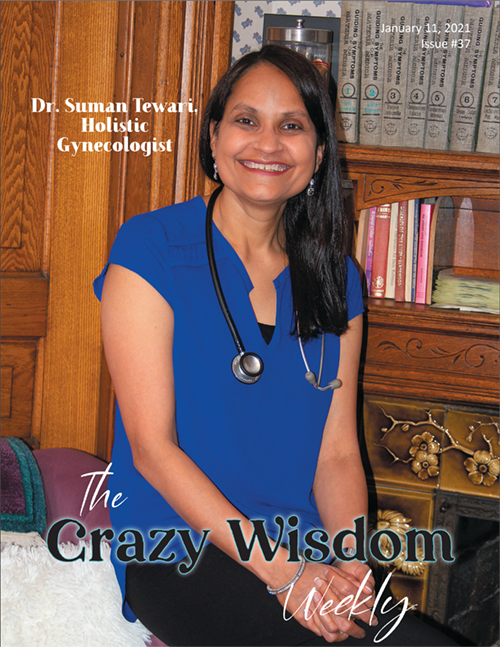























A graduate of Wayne State University Medical School, Dr. Suman Tewari is a women’s doctor who has incorporated many aspects of functional medicine and mindset coaching with her allopathic training to bring the best possible care to her patients. I sat down with her at her beautiful office in the Parkway Center to discuss what she means when she says “holistic gynecology” and why women might not feel “empowered to heal.”