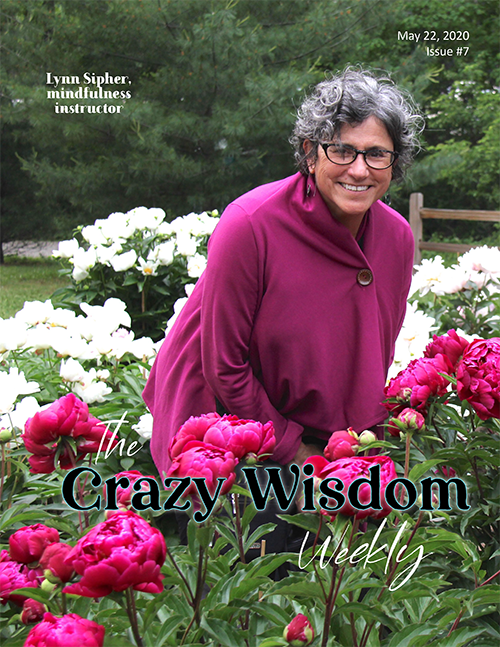
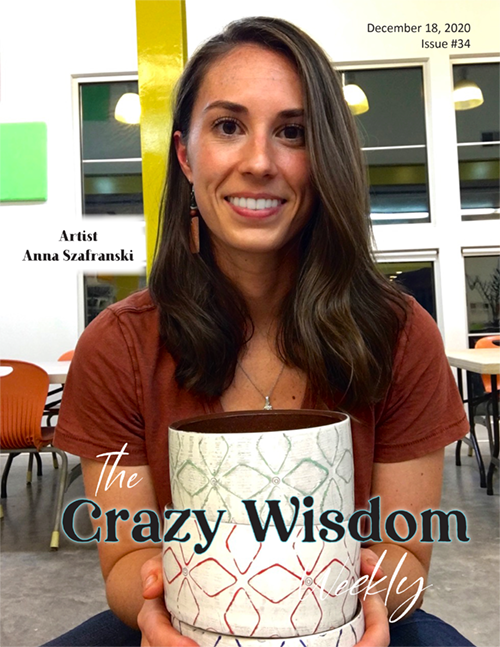
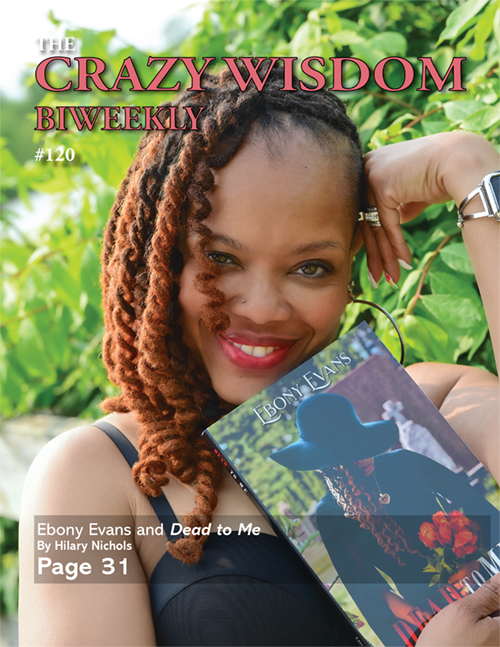
By Crysta Coburn. Photos by Susan Ayer
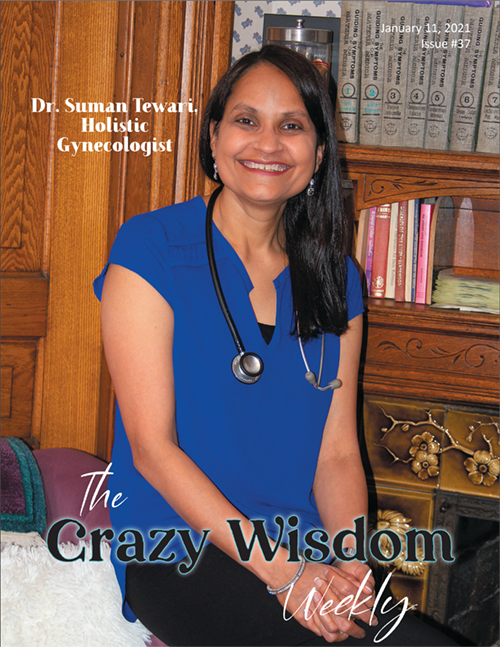
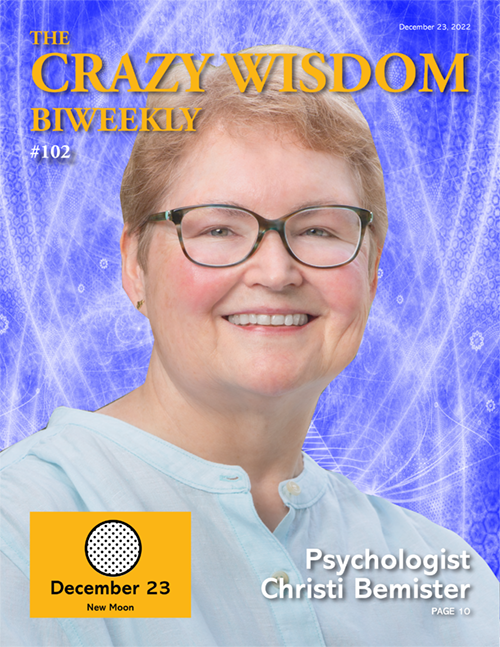
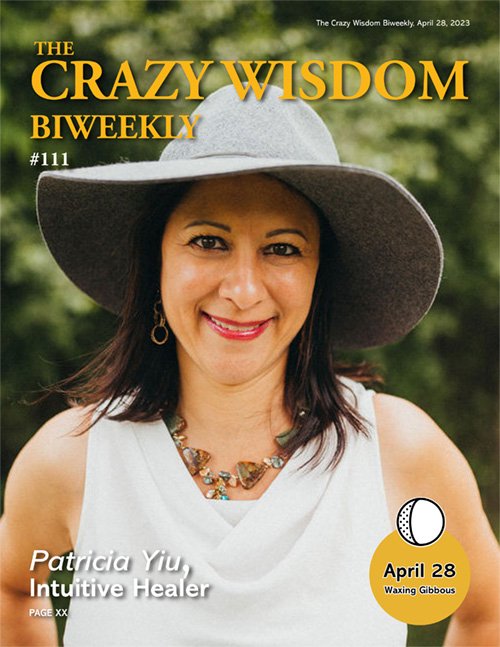
Dr. Suman Tewari
A graduate of Wayne State University Medical School, Dr. Suman Tewari is a women’s doctor who has incorporated many aspects of functional medicine and mindset coaching with her allopathic training to bring the best possible care to her patients. I sat down with her at her beautiful office in the Parkway Center to discuss what she means when she says “holistic gynecology” and why women might not feel “empowered to heal.”
Crysta Coburn: Please tell us where you were raised. Do you live in Ann Arbor? If you're comfortable sharing, please tell us your husband’s name and what he does, and your kids’ names and ages.
Dr. Suman Tewari: I was raised here in Michigan, on the west side of Detroit. And, yes, I live in Ann Arbor. I've been in Ann Arbor since 2014. My husband's name is Muneesh. He's a physician-scientist, an oncologist and researcher at the University of Michigan. We have two children. Our son, Vivek, is 14 and our daughter, Shreeya, is 12.
Crysta Coburn: Why did you choose to go into gynecology?
Dr. Suman Tewari: In the beginning, I wasn't even interested in becoming a medical doctor. I saw myself doing research on reproductive genetics and studying the process of meiosis (cell division in reproduction). One of the researchers in the laboratory where I worked was an MD. So, out of pure naïveté, I decided that I should get an MD to be able to do the research I wanted to do. I applied for medical school thinking I was going to get a combined MD PhD. But then, I fell in love with the clinical part during my third and fourth years of medical school and decided to focus my career on taking care of people.
When I got to my OB-GYN rotation, honestly, it was the deliveries that got me hooked. At the time, I didn't know what to call it, but I had what I know now to be a transcendental experience. When it came to the time of the delivery, even though there were many other people around—the attending physician, residents, and nurses—everybody was kind of just a blur, like they disappeared. It was just so amazing to watch this baby take its first breath. Being part of the process of guiding it out and helping it to enter the world was like nothing I had ever experienced. After the baby was born, everyone seemed to materialize back into the room again. I just couldn't shake that experience. And that happened for me with almost every delivery!
Crysta Coburn: So, that’s what led you down the path of specializing in obstetrics and gynecology?
Dr. Suman Tewari: Yes, but once I got into private practice, the real-life stress of all the responsibility that I never had as a medical student or resident weighed heavily on me. The years of disruptive emergency calls and deliveries at all times of day and night wore me down. Ultimately, the high price of malpractice insurance for obstetrics made it easy for me to stop delivering babies. Once I narrowed my practice to gynecology, I experienced another thing that was totally unexpected: I realized that I was only treating patients at a superficial level, addressing symptoms, but not the underlying causes. That was a tough realization for me because it went against the grain of all those years of education, training, and clinical practice.
It was a disorienting period of time. I went on a journey of deep soul-searching. I hired a coach who helped me restore my sense of who I was and to build the confidence that I needed to break free and try something different. That's when I discovered functional medicine, which takes a holistic, integrative approach to medical care. And a holistic approach is something that makes good common sense to me. There's no way I could ever go back.
CC: Why integrative? What do you mean by using that particular word?
ST: What I really mean by integrative is addressing not only the physical, but also the mental, emotional, and spiritual aspects of an individual, to heal at multiple levels. You can’t fully heal the body without taking these other elements into account, because they are all interconnected. For example, in my conventional allopathic practice I often treated biochemical abnormalities, but didn’t really ask...why is the biochemistry off. Now, I routinely ask this question, and it often leads me back to what's going on with inner thoughts and beliefs, because these run our lives.
An additional meaning of integrative is being open to other healing approaches beyond the conventional allopathic model that I trained in. There are so many other ways of healing practiced all over the world—traditional Chinese medicine, ayurvedic medicine, homeopathy, acupuncture, and many more. Allopathic medicine is important and can be lifesaving for acute emergencies, as well as for other conditions. Yet there are a number of chronic health challenges where allopathic medicine falls short, where it only treats the symptoms and doesn’t get to the underlying cause. With an integrative approach, our intention is to search for that root cause. And it's not always easy. It depends on the person and how far they may want to go. How much healing do they really want?
CC: So, what you mean by integrative is holistic. Healing the whole person.
ST: It is! It’s holistic, [healing the] mind-body-soul [simultaneously], absolutely. Life events can have a major effect on physical health, and most of us are not taught how to deal with our emotions in a healthy way. For example, a woman who has gone through a divorce and not healed emotionally could experience physical symptoms even years later. We need to not only address the physical symptoms, but also address the emotional disturbances to heal fully.
Our body is always working for us. It's always trying to keep us at our optimum. And that's one of the key things I try to let the patients know when they come here—to be thankful for your body, because it’s taking care of you. Like, okay, I want some of this weight to be gone. But wait, body, I see that you’re doing your job well, to keep me alive. Even when I put excess food in you, you adapt to it and store it away for me. It’s seeing how much your body is doing for you at all times. When I think that way, I don't have to force myself to eat better. If I have a loving relationship with my body, I want to take care of my body, right? So, you have to be grateful for the body that you have. Otherwise, we're just upset with the body, and that energy doesn't help. Love is usually the answer. Loving yourself and loving your body.
CC: What kinds of results are you seeing compared to a straight allopathic course?
ST: One of the common things I hear from my patients is that they feel empowered. Although this is starting to change very slowly, in the traditional allopathic model, patients are placed in a passive, rather than active role. In the holistic model that I prefer, the physician is a facilitator of health, not the ultimate authority. For instance, I encourage my patients to tap into their intuition when it comes to making choices about various options and alternatives for treating a particular condition. That more expansive mindset carries over into other areas of their lives as well.
I've also noticed that the women I take care of develop a different relationship to their bodies. They better understand their bodies and are better able to tap into the vital connections between their heads and hearts and everything else in-between. They realize that this is a journey of healing. It's not a “one and done.” They don't expect to lay down on the exam table and walk out with a quick fix. They take better care of themselves. Because they are more in tune with what's going on with their bodies, they are more proactive about their health and well-being. Having my patients take a proactive role in their health helps me to be a more effective physician. And it's a more satisfying way for me to apply my knowledge, skills, and experience.
CC: You talked about being better in balance. How do we become better balanced?
ST: It starts with accepting ourselves for who we are, where we are, as we are, and giving ourselves permission to be that way, whatever way that is. So, we're not resisting and fighting. It's not about not having wants, it's great to have wants, and goals, and desires. But it's not [great] to be coming at it with this resistance energy, energy of “it should be a different way, it shouldn’t be this way, I should be ten pounds lighter,” whatever it is. And instead of that, it's having the attitude that this is great what I have, but I’d like to be this way. What can I do, what's in my power [as a health facilitator] to do that's going to help you get there?
What I've experienced is anything that brings you joy and calmness, that's what's going to help you. So, when you're asking yourself, what do I do? How do I get myself in balance? It's about how do I get joy flowing in me? Usually there’s nervous energy, or there’s something in the past. You could be unbalanced on many levels. It will manifest itself, physically, your blood pressure is off balance, but it's actually happening at a deeper level. What is off is I have a desire that’s not meeting my current state, we’re not happy with our current state. That's not a bad thing. That's actually a good thing. That's feedback to you that, hey, we could be doing better. We have a goal, and maybe the goal is a little too much. Maybe we need to make a smaller goal. Instead of saying, “I want to lose 50 pounds,” maybe five. It just becomes more attainable, and it calms you down. Anything that calms your nervous system down is going to be better for you and is going to help you get back in balance.
This is where I get into adrenal health. To me, the adrenal gland gets very little respect in the medical world. In the allopathic medical model, unless you're way off—your cortisol is way high or way low—there's no treatment for it. We talk a lot about the sympathetic and the parasympathetic nervous system, sympathetic being the fight or flight and parasympathetic being rest, relax, and restore. You are faced with a traumatic situation, and boom. Your adrenaline kicks in. Your cortisol has to rise. You’ve got to get away from the situation, or you’ve got to deal with the situation. You’ve got to be armed. That’s where our bodies need to be at that time. The problem is, we don't know how to shut that off very well afterward. And then when we’re replaying it [in our heads], we’re still in that fight or flight moment. And we're faced with that a lot on a daily basis.
I won’t say this [is true] for everybody, but most of us are “on” a lot during the day hours. The only time we're really “off” is probably during our sleep hours. And many people are not sleeping well. They may go to bed, but are they really sleeping? Getting good sleep and getting the rest that you need is where the real healing takes place, because that's when your body is at work getting everything back in balance. During the day, because we're on so much, we don't have enough down time. Unfortunately, we're on, and it's like being on the whole time, then we wonder why we're depleted, why our cortisol levels are off, why we’re gaining the weight, why the sugar is off, why there is a blood pressure problem. I feel like a lot of it is just from that [depletion]. The more we take care of our emotional health, the more it translates into more life. Learning how to deal with life, and realizing that, [whatever issue we were dealing with] is not the end of the world may help us activate our parasympathetic (rest, relax, and restore) nervous system more and bring us back into balance.
I don't want to set people’s goals, but the majority of us agree the goal is to be happy—to have joy. I like to think about what that really means. What’s it like to be joyous? You're actually enjoying life. Life isn't meant to be miserable. And I don't think we realize often enough that we’re miserable because we're not taking the time to ask [ourselves], “Hey, how much joy do I have in my life?” But that is a question I ask myself more and more as I've been on this path. I'm evolving all the time. That's been my most recent question before going to bed. How much joy did I experience today? What filled my cup of joy? That leads into the gratitude journal. I advise a lot of my patients to do this. Before you go to bed, be thankful for all the things that went right. First thing in the morning, be grateful that you have another day. Start appreciating the things we already have and are taking for granted now.
CC: How do you help your patients become better balanced?
ST: I work on it from different angles. Depending on what’s going on, I may need to evaluate their hormonal balance, to coach them to help balance their perceptions (mindset), and often also work with them to discover what activities will help them feel more in balance. It’s different for different people. We live in a wonderful age where it's so much more acceptable to take time for yourself. For some, it’s yoga and meditation. It could mean doing an Epsom salt bath. Go and soak in a tub for half an hour—whatever is joyous. Often, I find that we as women need to give ourselves permission to do less. We are so much about evaluating our worthiness based on how much we do. Last I checked we were human beings, not human doings.
CC: What can a woman expect on her first visit with you?
ST: My interaction with a new patient starts with the first phone call. I want to get to know her and to see if this is really the right fit for her. I haven't done much marketing yet, so most women reach out after hearing about me from other patients or being referred by their doctor. At that first visit, the goal is getting to know her, to understand how she operates, and who she is. The key thing is that women have the answers within them—the healing happens from within. And I listen, not judge. A lot of things are being said, and it’s not only what’s being said, but what’s not being said that I pay attention to. These are clues. The answers are there, and I help bring them to the surface.
She can expect a visit that is very different from what she may be used to. A new patient visit is typically an hour and a half in length, in which I not only review her medical history, but come to know and feel who she is as a person. Sometimes this involves a physical exam, and other times that part doesn’t happen until a second visit. A new patient can expect to be received by me as two people in one body—as both a gynecologist medical professional, and as a woman. She can expect to be received not just as a patient, but as a person. She can expect to be heard, and that I will work with her to also uncover the things she is not saying, that she is not asking, but which matter greatly to her and her healing.
CC: Do you ever find that women aren’t used to being listened to?
ST: I think there is a lot of truth to that. I think it’s that they don’t feel heard, not just what they say, it’s what they’re not saying. And for whatever reason, I can tune into that. Maybe it’s because I’m interested in what’s happening on a deeper level. I always want to know why things aren’t working. Just because something has worked for ten people, doesn’t mean it will work for you—I believe you! People are not lying. If they say they’re in pain, believe them. They’re in pain if it’s at the mental level or the physical level. Just because I don’t know what’s going on, doesn’t mean it’s not happening. That’s healing itself, just being heard.
CC: Do you integrate use of herbs and supplements? Especially, with regards to menopause?
ST: Yes, I do. I think this is an important aspect of the holistic, functional medical approach.
There's so much that can be accomplished naturally or with herbs and supplements for menopause, even without using any hormones directly. For example, black cohosh (an herb) and Siberian rhubarb (a vegetable) have been found to reduce the frequency and severity of hot flashes.
Most people don't realize that adrenal gland fatigue can worsen the symptoms associated with menopause. So, when I'm working with a woman who is perimenopausal or in full menopause, supporting her adrenal glands is one of my top priorities. I frequently recommend adrenal support supplements such as licorice root, ashwagandha, and ginseng along with daily exercise, staying fully hydrated, regular meditation, breathing techniques for relaxation, and making a concerted effort to improve one's quality of sleep and rest.
CC: What is the age range of the women that you treat?
ST: The youngest patient I've seen was a 10-year-old. I have patients in their 80s. But the majority of the women that I'm taking care of are between 20 and 70.
CC: Can you give some more examples of the issues of menopause and perimenopause that you address holistically?
ST: Women going through perimenopause and menopause commonly experience hot flashes and night sweats, mood swings, trouble sleeping, painful sex, dry skin, thinning hair, weight gain, as well as aches and pains related to joint stiffness. The knee-jerk approach from the allopathic model is to prescribe hormone replacement, antidepressants, and other synthetic drugs. While these have their appropriate time and place, as you might expect, I take a different approach.
As I've mentioned earlier, I recommend a variety of natural remedies for hot flashes and night sweats. I've mentioned the connection between adrenal health and menopausal symptoms as well. Adequate hydration is important for helping your body wash away harmful toxins and keeping your joints working as smoothly as possible. For more restful and rejuvenating sleep, I recommend establishing a calming, relaxing routine before bed, including things like:
Taking a bath with essential oils
Reading uplifting material
Writing in a gratitude journal
Prayer
Guided meditations and breathing techniques
I also recommend putting away electronics to bed 30-60 minutes prior to you turning in for bed.
Nothing beats regular, vigorous exercise for at least 30 minutes a day, at least several times a week. In fact, multiple studies have demonstrated that such an exercise practice is more effective than prescription anti-depressants for elevating one's mood. The only problem is that exercise doesn't come in a pill!
Now here's the thing that I believe is a really important aspect of a holistic approach to menopause: I see this period of a woman's life as an opportunity for deep personal growth. It's an opportunity for a woman to explore previously unexamined beliefs, patterns of thinking and decision-making, and habits of taking action. All of this has been ingrained from decades of being on "autopilot." Such beliefs may have served a woman well at one time, but no longer; in fact, they may now be having a negative affect.
It's also an opportunity to challenge the results of one's previous choices and actions. Such as the health of your home and work environment, and the health of your relationships. I encourage my patients to adopt a flexible attitude and mindset of going with the flow of life.
In my estimation, maybe about 5-10% of women that I've seen experience menopause like this: "Oh, my last period was 12 months ago, and you know what, I have no idea about what a hot flash is like." The interesting thing about these women is a pattern I noticed—all of them take life just "as-is." They see the positive sides of things. They accept what's so. They don't struggle in their minds (and, therefore, in their bodies) with "shoulda, woulda, coulda" self-talk. Now, they're not passive by any means. Rather, they have an "attitude of gratitude." They're grateful for the opportunities to grow, they embrace life's challenges.
I don't want your readers to think there's something wrong with them, that there's something automatically wrong with their mindset because they are experiencing menopausal symptoms. Instead, I think it's really, really important to provide a lot of reassurance to a woman who is going through this. It can be a scary time, keeping fears and concerns bottled up like, "Am I normal? Am I still attractive? What do people think of me? Am I still going to be able to do the things that I enjoy? Is there something wrong with me because I feel the way I do? I've read things about other women, but is what I'm going through, okay? Am I odd?"
Real related article: The Healing Power of the Right Relationship: How Elizabeth Shadigian, M.D., and WomanSafeHealth Are Raising the Standards for Women's Health Care
As you might imagine, so many of the emotional and mental concerns that come up don't get expressed. For many women, there's no safe place to do so. That's my approach, it starts with listening and reassuring. A lot of it. So much is happening physiologically, mentally, emotionally, even spiritually. And it's easy to misinterpret things they've heard and read.
About a year after I stopped delivering babies, I had this epiphany: I am helping women with birthing their new self, the next version of their self-expression and freedom!
CC: That’s beautifully said! Though you are not an oncologist, as an integrative gynecologist, how might your approach differ when you are working with women with breast or ovarian cancer?
ST: My approach starts with the basics, assessing their overall health, regardless of what illnesses and diseases exist. I'm looking for root causes of their condition. So, some of the questions I ask are:
What is important to her in her life? (values, meaningful)
What is the level of inflammation present in her body and what can we do to cut down her inflammatory state?
Is her immune system over- or under-active? What can we do to boost or calm down her immunity?
How can we improve her gut health?
What needs to be done as far as detoxifying the body?
What are her religious and spiritual practices, if any?
What lifestyle factors can be improved? (Smoking, drinking, drugs, exercise, diet, relationships, friendships, work, sleep)
What dietary and nutritional factors need to be considered?
What hormonal imbalances exist and need correction?
What's her home and work life like?
Is she in healthy, supportive relationships?
What emotional factors contributed to the cancer? Do they still exist?
You know, in traditional allopathic medicine, the contribution of emotions is, unfortunately, ignored for the most part. But we know that our emotional states influence our physiologic states. When we're excited or scared, our heart rates go up. When we're relaxing or meditating, our heart rates go down. So, what's happening at the cellular level? A lot that we don't know about or understand yet!
To help address inner conflicts that can affect my patients’ health, I provide mindset coaching as part of my approach. We often work on emotions, beliefs, fears, and concerns as they relate to their lives, in general, and medical conditions, in particular.
I also think self-love and learning to appreciate who you are is important. Only then can true healing begin. Self-loathing and negative self-talk contribute to depressing the immune system and other cellular processes that are vital to optimal health and well-being. All of this makes sense when you hear it and read it, but in practice it’s more challenging. I support them in developing the habit of valuing and validating themselves, by doing things for themselves. Sometimes this means pursuing interests that they've pushed away for years, for instance.
Relationships are important to consider as well. But also, often overlooked. Cultivating healthy relationships and healing conflicts—whether it be with a boss, a spouse, a kid, a parent—it takes a lot of work. But it's an investment of "heart" dollars that pays a lifetime of dividends.
CC: Many women have fibroid tumors. Please talk about ways that you might approach this that would be the same and would be different from a strictly allopathic gynecologist? With UTIs (Urinary Tract Infections)? With STIs (Sexually Transmitted Infections)?
ST: Fibroids are the result of a hormonal imbalance where there's too much estrogen in her system, relative to the other hormones. A woman with fibroids needs help with clearing estrogen out of her system.
In my allopathic training, time was the issue, there was no discussion regarding the underlying cause. Basically, we were taught to either manage it with hormones (birth control pills, progesterone, or [hormonal] IUD) or, if they were symptomatic with persistent bleeding or pain, then we took them to surgery, and you removed it and—voila! You fix their pain and bleeding issues, but you never addressed what was the original cause of it, so they're still running around with that imbalance in their hormones!
To balance their hormones, one of the things to do is, yes, you can give them the progesterone to help offset the extra estrogen in their system. But the other thing I like to focus on is studying how they are processing the estrogen in their bodies and getting rid of the estrogen. This is important to consider because there is a healthy way and an unhealthy way to metabolize your estrogen. By understanding this, I can give them supplements to help them process estrogen in a healthy way and get rid of unhealthy, harmful forms of estrogen before they can cause any long-lasting damage.
When treating UTIs, one of the things I do differently is to focus on improving the healthy bacteria that live in the genital area and urinary tract. This is called the microbiome. There is a probiotic that women can take that is specifically designed to improve the health of the tissues that line the bladder and vagina. For women who are prone to UTIs or vaginal infections, I've observed that taking this probiotic daily helps reduce the likelihood of getting an infection. For women who have an active infection, I start them on the probiotic as well. It's also important to consider their nutritional status, in particular, levels of certain vitamins, like B12, folate, magnesium, and other micronutrients. I help patients sort this out by ordering a nutritional profile.
For STIs, it's a matter of boosting their immune systems, which I address more now. I didn't learn that in my allopathic training. If I am treating a patient with antibiotics, I recommend that she also take probiotics to help keep a healthy balance of healthy bacteria in her gut. It's common knowledge that antibiotics are going to affect your gut microbiome, but even so, some doctors still overlook the importance of taking probiotics along with antibiotics.
In contrast to the allopathic model, I think it's important to address the emotions associated with dealing with an STI. It's one thing to write a prescription and hurry a patient out the door. But to really help a patient, I think it's important to discuss the health of their relationships with lifestyle choices and sexual partners. It's also important to acknowledge that their self-esteem can be negatively impacted by contracting an STI. Just mentioning this to a patient can give her a sense of relief from validating her feelings, like guilt, shame, and fear. It's important for her to be heard, even if she doesn't want to discuss it much further.
CC: Thank you so much, Dr. Tewari! It has been wonderful speaking with you.
Dr. Tewari can be contacted at DrTewari@A2HG.net or by phone at (734) 418-2188. Visit her online at annarborholisticgynecology.com. Her office, Ann Arbor Holistic Gynecology, is located at 2345 South Huron Parkway in Ann Arbor. She is seeing patients both in person and by telemedicine.








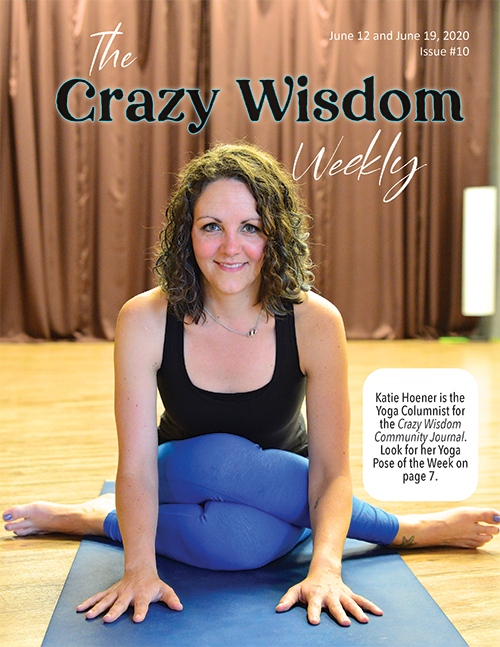















And so, many years ago in a plane, 40,000 feet above the ground, the woman guided Tull through a couple of basic yoga breaths and stretches. “I felt 200% better,” Tull recalled, still obviously in awe at the transformation.