By Judy Stone
In the early 1990’s, when first beginning my foray into nutrition work, the cutting edge was the emergence of the low carb diet. The Atkins Diet was published in 1992 and faced off against the high carb, low fat heart disease reversal program of Dean Ornish. Ornish is a physician who led the public and the medical community toward a plant based, low fat lifestyle approach to preventing and reversing heart disease. Previously, author Adele Davis, (Let’s Cook It Right published in 1947 and Let’s Eat Right To Be Fit in 1957), was one of the early, well-known pioneers to put forth the idea that what we eat is directly related to health and that by “eating this and not that” we can exercise a measure of control. Three plus decades later in my career, we’ve wound our way into an increasingly more sophisticated, nuanced, complicated, and confusing world of knowing how to feed ourselves. Food, supplements, and nutrition advice (including apps) is an industry somewhere in the hundreds of billions of dollars annually. We are now squarely in the age of personalized nutrition, and yet, attaining and maintaining good health throughout our lifespan, has never been more challenging.
Too many people are more ill, and many are fearful and/or traumatized around food and what and what not to eat. The truth is food can make us unwell as much as it can improve health. It’s become harder, more complex, and more expensive to nourish oneself, and those without the resources to access more and healthier food options, health care, and nutrition guidance likely suffer the most.
We face an increasingly complex array of health conditions and food intolerances (perhaps known but often not) resulting from genetics, underlying imbalances driven by environmental toxins, gut microbiome imbalances, epigenetic alterations (gene changes driven by interactions with environmental factors, both internal and external to our body), pharmaceuticals, and yes, even stress and trauma. Many people’s lives are affected, if not dominated by any combination of persistent or frequent pain, digestive disorders, skin conditions, chronic fatigue, chronic mental health struggles, diminished cognitive function, tinnitus, tachycardia, autoimmune disorders, body temperature dysregulation, sleep disturbances, anxiety attacks, and more, in addition to the standard array of chronic diseases. Many of these problems can be triggered or exacerbated from eating the “wrong” food. But it may not be apparent what the “wrong” food is, at least not without some detective work. Paradoxically, the idea that “food is medicine” can morph, much like our genes, into “food as toxin.” Whew.
One Example: Histamine Intolerance versus Mast Cell Activation Syndrome
Over the last decade one culprit for the complex and variable combinations of symptoms and illnesses, the mast cell, has received an increasing amount of attention. Mast cells are white blood cells that hang out in tissues throughout the body, especially in the gastrointestinal tract. Their function is to set off inflammatory responses to protect the body in the face of injury or infection by releasing pouches full of chemical mediators. The most well-known and understood of these is histamine. Most people are familiar with antihistamine drugs used by so many to control responses to outdoor allergies or asthma; these drugs are specifically mitigating the effects of massive histamine dumps by mast cells. There is growing recognition that many people either have mast cells that are over reactive and producing too much histamine or have an overabundance of mast cells also leading to too much histamine being released. In addition, the main enzyme the body uses to degrade histamine, called diamine oxidase or DAO may be in short supply, making it difficult for the body to break down histamine. Low levels of DAO can be due to a genetic variant, deficiencies of nutrients needed to make DAO or to help it work, or gut problems in the small intestine, where DAO is made, thus inhibiting production.
There are multiple types of mast cell disorders not covered here, but two prominent categories are Histamine Intolerance (HI) and Mast Cell Activation Syndrome (MCAS). HI is a problem of mast cells overreacting in response to higher histamine containing foods and insufficient DAO enzyme production or function to keep up with breaking it down, while MCAS is a problem of having too many mast cells, which also are overreacting with histamine and over two hundred other chemical mediators. MCAS manifests differently in different people, but one of its defining features (diagnostic criteria) is that it involves symptoms across at least two body systems and organs happening at the same time in response to stimuli, which could be food or non-food stimuli. MCAS is also less common than “garden variety” histamine intolerance.
Read related article: Enhancing Detoxification
Does any of this sound familiar?
Unfortunately, there is no one picture to point to, to say this is MCAS or this is HI. Of the two, HI is less complicated, and symptoms can be similar to those one might experience with allergies—congestion, headaches, hives, rashes, exaggerated responses to bug bites, poison ivy etc. But it can also manifest as fatigue, brain fog, vertigo, anxiety or difficulty concentrating. Symptoms theoretically are more pronounced in the hours or day after eating a meal with a significant histamine load but since most people are frequently eating a lot of histamines because it’s not something most people think about, symptoms may seem constant and just part of life until dietary histamines are reduced. Histamines can also be triggered to environmental exposures to dust, mold, etc.
For people who have been chronically ill long-term, with problems affecting multiple body systems as noted above (e.g. GI complaints, temperature dysregulation, insomnia, anxiety, etc.) and for which no other explanation has been found, consulting with a functional medicine trained physician with MCAS experience may be worthwhile. While definitive diagnosis thru testing is difficult, identifying the possibility of MCAS when no other diagnosis for chronic, multi-system symptoms have been found, could be useful in leading to treatment of all the underlying problems that are creating havoc.
In either suspected HI or MCAS, following a low histamine diet can often be helpful preliminary detective work because it will lighten the histamine load in your body and may reduce symptoms. However, it’s important to realize that many things can cause histamine to dump—anything that triggers the immune system. A good starting point for identifying histamine levels in food can be found in the free app called Food Intolerances. Usually sticking with low histamine foods for a week will provide noticeable results if HI is the primary problem. Histamines are especially high in fermented/pickled foods, alcohol, citrus, chocolate, tomatoes, eggplant, green beans, chili peppers, vinegar, aged cheeses, smoked and aged meat, or leftover animal protein (over 36 hours). This is not a definitive list; there are also foods that “liberate histamine” and foods that inhibit DAO enzyme production. But it’s a good starting place.
New Tools for New Times
If this seems confusing, it’s because it is! Histamine intolerance or MCAS are but two examples of complex problems receiving more attention of late. It’s important to realize that food is not the origin of these problems, but dietary strategies can help alleviate symptoms and help address the underlying drivers of the problems. While nutrition is core to health, we each have unique genes, biology, and biochemistry and each person’s history, including trauma, drug/chemical/toxic exposures, stress and food history all play a role in shaping health and health needs. All of these need to be considered as part of a healing strategy. As healthy eating means different things for different bodies and at different life stages, we fortunately have more research, tests, and tools than ever before to help personalize diets to fit the individual and their current health, food, and nutrient needs. The goal is not to live with limited diets, rather to fix underlying issues, increase the body’s tolerance for a wide range of healthy foods, and live with more health and vitality.
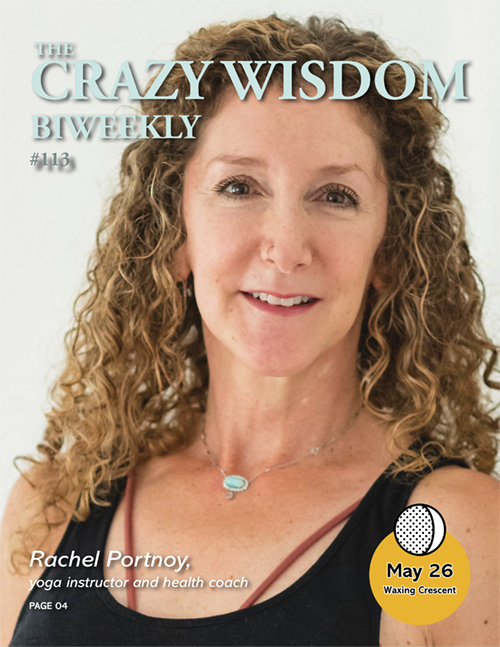
Judy Stone MS, MSW has worked in the community for over 30 years—first as a psychotherapist, then as a nutritionist. She has a master’s in human nutrition from a functional medicine/nutrition perspective from the University of Bridgeport. Stone has a limited private practice working with older adults, and volunteers doing nutrition education for underserved communities. Learn more at CenterforFunctionalNutrition.com.











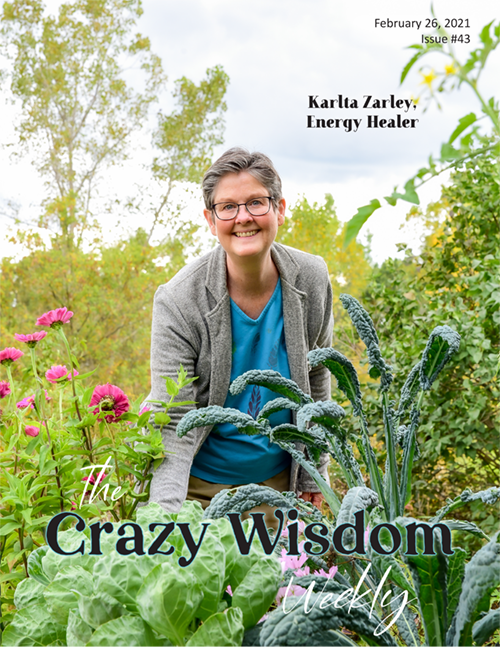







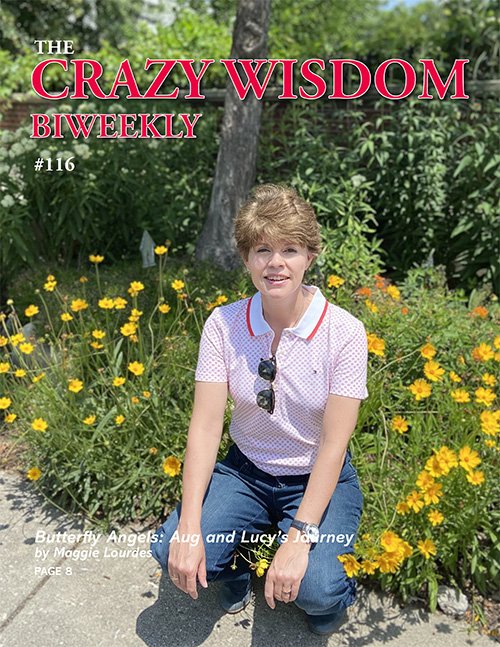




A community garden is like a little shared oasis, a special spot where folks from all walks of life come together to grow delicious veggies, fragrant herbs, and beautiful flowers. It becomes a green sanctuary, where members roll up their sleeves, dig in the dirt, and let nature work its magic. Often organic, community gardens help promote soil health and community connection as much as they do delicious, locally grown food.