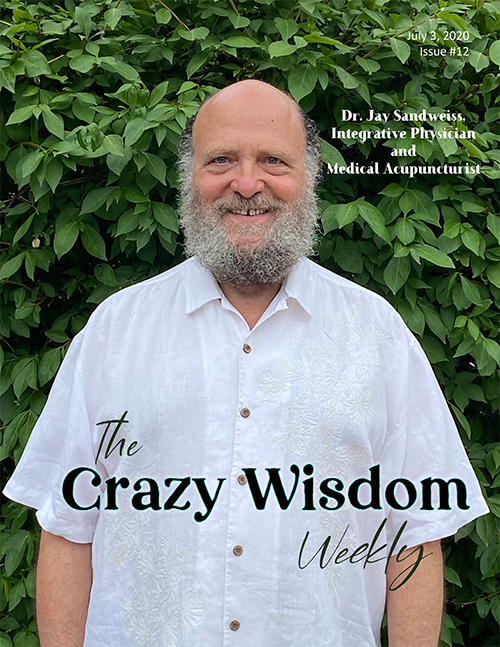
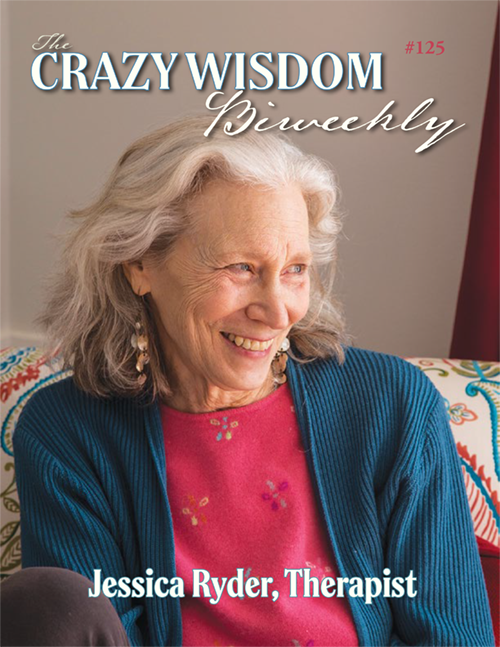
Interview by Bill Zirinsky
Photography by Mary Bortmas
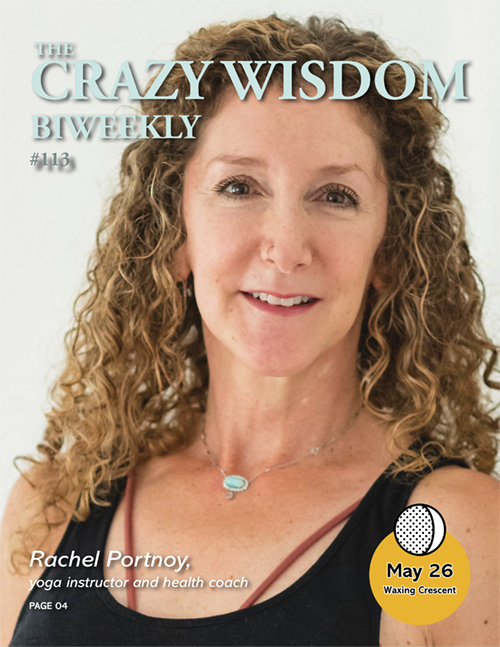
Dr. Amy Saunders is one of the leading integrative medicine doctors in the area. We had profiled her ten years ago, and we wanted to check back in with her, and see how she had viewed Covid, and hear her current points of view on her medical practice and providing integrative care. We also were hoping to talk with her about the influences which shaped her becoming the attuned, committed and deeply caring physician that she is known to be.
Dr. Saunders was born and raised in Findlay, Ohio, and lived there through high school. She went to Kenyon College for 2 years, and completed her BS and MD at Ohio State, and she also completed her Internal Medicine residency there. Additionally, she has a master’s degree in Public Health from the University of North Carolina.
Dr. Saunders focused on patient care and teaching during her 20 years on the medical staff at University of Michigan Hospital. She then went into her own private practice, Integrative Healthcare Providers (IHCP) which is located on South State Street near Briarwood Mall. As she explains in the interview, the practice is a collaborative one, and there are a variety of other integrative health care practitioners sharing the same office.
Dr. Saunders has been married for 43 years to David Rooney, whom she met in high school. They live in the Lansdowne neighborhood of Ann Arbor. They have two daughters. Their oldest, Kate (33), lives in Ann Arbor with her husband, Cade Sperlich, and their young son, Ellis. Their younger daughter, Liz (28), lives in Ypsilanti.
In person, Dr. Saunders is soft-spoken, attentive, reflective, and easy to enjoy talking with. She smiles readily and has an elfin twinkle in her eyes. She loves getting together with her family, cooking together, and playing games. Her “guilty pleasure is watching college football in the fall and rooting for the Ohio State Buckeyes (though our Kate does not understand this).”
Bill Zirinsky: What is incorporated into your sense of integrative medicine and integrative health care?
Dr. Amy Saunders: There are so many modalities and approaches to care that can be beneficial! It is simplest to outline some of the modalities I incorporate by the kinds of health problems they can benefit.
Musculoskeletal pain: My first experience with realizing how effective nonallopathic modalities can be in treating health problems was through my work with physical therapists taking care of mutual patients with chest pain, back pain, and headaches. Many PTs in Ann Arbor do a great deal of manual therapy – realigning vertebrae, ribs and pelvis and other musculoskeletal regions that can cause extreme discomfort when out of balance. I think malalignment is a cause of a great deal of pain and disability that is underrecognized by most allopathic providers. Unlike many physicians, for me it was a logical step to go from appreciating what PT’s can do to appreciating chiropractic skills and massage therapists’ skills. I have also observed that craniosacral massage is helpful for many patients who have suffered even minor trauma and who have persistent unexplained neurologic or musculoskeletal symptoms.
I also use light therapy, also known as cold laser or LED treatments for both musculoskeletal problems and for wound/fracture healing. It can also be highly effective in helping to relieve muscle spasm. I first learned about that modality from a local veterinarian, as vets use it far more than allopathic providers, even though there are lots of well-designed research trials documenting its efficacy. The fact that the FDA has still considered it experimental therapy and insurance does not cover it is a testament to how biased toward the pharmaceutical industry they are, unfortunately.
Metabolic imbalances: I use herbal therapies or biologic supplements in situations where there seems to be either metabolic imbalance or high levels of inflammation. Philosophically, I have come to appreciate that trying to figure out how someone’s body is out of balance is generally much more useful than trying to find a disease diagnosis label. And each of us can get out of balance in our own unique ways based on genetic, environmental and lifestyle factors. Diagnostically I utilize some functional medicine testing to try to determine what is out of balance in the individual patient. For example, stool tests that are unavailable in the allopathic medical setting -- tests that look at markers of inflammation and the health of the microbiome -- can be invaluable in helping a person get back in balance. In addition, nutritional assessments, including nutritional markers and sometimes food sensitivities, can be very valuable in directing healthcare and advising diet/lifestyle adjustments. A healthy diet is probably the most important factor in maintaining health, and a much more important source of balanced nutrients than a boatload of supplements.
Inflammation: There are many clinicians and researchers of all stripes who believe that inflammation lies at the center of most chronic health problems, either as a trigger for illness or as secondary effect: diabetes, coronary heart disease, cancer, dementia, peripheral vascular disease. As a global theory of inflammation as cause of illness the idea is that the body responds to chronic inflammation – whether it is low grade gum inflammation or the lining of the gut for example – the body responds with a cellular response that increases production of inflammatory molecules – that can lead to membrane and intracellular injury in other parts of the body. Therapeutic approaches to reduce inflammation primarily involves avoiding toxins and maintaining an anti-inflammatory diet. In addition, advising use of supplements that have anti-inflammatory effects such as turmeric, quercetin, boswellia, and others when appropriate can be very helpful.
In terms of diagnostic methodologies, the kind of testing we utilize in addition to allopathic pathology lab testing often aims to measure active cellular or organ processes – hence the name “Functional Medicine” testing.
For instance, GI function tests measure presence of inflammation, assesses digestive markers, and the health of the microbiome, the bacteria in the gut. This test provides way more information than available allopathic lab tests.
Adrenal functioning can also be measured in a much more useful way than what was available to me at U of M, looking at cortisol changes through the day as well as the ratio between cortisol and other adrenal hormones that address the issue of whether chronic stress has been taking a toll on the adrenal gland.
Methylation Panel and genetic testing is at a more advanced state through independent labs like Genova Diagnostics and others than it is at U of M and other academic labs. While we have to be careful to make sure we are not placing too much certainty or getting too specific about our test conclusions, I am confident that these functional medicine tests provide valid information that allopathic medicine will adopt some time in the future, just as they have adopted tests for small intestinal bacterial overgrowth and leaky gut. I feel fortunate to be able to make the choice to use these tests now.
But to be honest, in this process of trying to help someone, I often try to use my sense of intuition, which I believe is one of the most important tools that any person in a healing profession has. Our tests are not perfect and our understanding of them is even farther from perfect. I describe myself as the “queen of empiricism” because, in most cases, the approach that we take (the patient and I, as a team) is one of “let us try this and see how you do. If that does not solve the problem fully then we can talk about what other steps we can take.” That is the strength of both integrative medicine and primary care – time can be an ally in finding solutions. My intuition and sense of what may be out of balance may also lead me to recommend different things – like walking in nature, meditation, singing, journaling, or even encouraging addressing grief or conflicts within one’s family, for example. That is another strength of practicing integrative medicine as a primary care provider: when you have a longstanding relationship with a patient you can better understand how their life affects their health.
I also refer to my colleagues who practice Traditional Chinese Medicine, acupuncture, ayurvedic medicine, massage, and many forms of energy medicine such as Reiki, polarity, Healing Touch, trauma touch, reflexology, and others. I cannot begin to express my respect for them and the ways that they help people heal. As I get older, I have an ever-growing appreciation of the fact that there are ways of knowing and healing that I only have a superficial understanding of.
Bill Zirinsky: Can you tell us about the other practitioners in your clinic?
Dr. Amy Saunders: At Integrative Health Care Providers (IHCP), each of the practitioners has her/his own panel of patients and integrative care approach and that is one of the greatest strengths of our clinic, I think. I am an internist and see only people older than 15. Drs. Amanda Dakroub and Sean Zager are Family practitioners and are both Board-Certified in Integrative Medicine. Dr. Dakroub has a large primary care practice with a very broad range of knowledge about integrative modalities. She also has a substantial number of transgender patients. She is one of a fairly small number of primary care practitioners in the community who is very experienced in pharmacologic and psychosocial care for that population and works in collaboration with the Comprehensive Gender Services program at U of Michigan.
Dr. Zager is the only male physician in our clinic and has a special interest in providing integrative care for men. He also has extensive experience in evaluating and managing functional GI abnormalities. He has conducted some educational programs for patient groups, where information and patient experiences can be shared to enhance understanding.
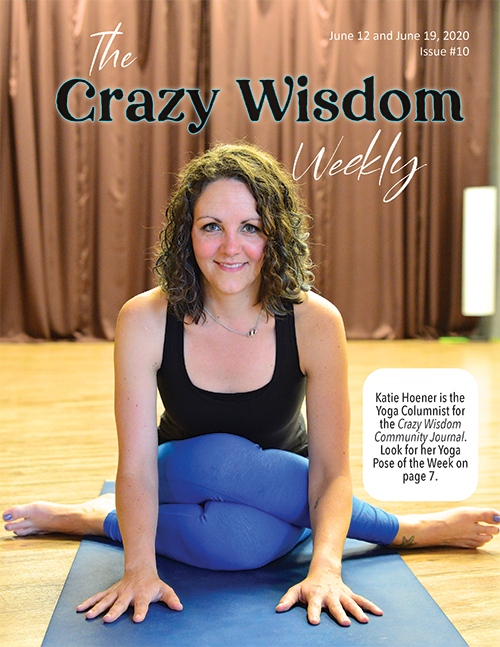
Dr. Wendy Luo is a Physical Medicine and Rehab physician who is also trained in integrative medicine and has expertise in acupuncture for pain relief and uses integrative approaches for management of headaches, chronic pain, insomnia and for weight loss.
We also have two excellent nurse practitioners, both of whom have certification in adult general primary care. Brenna Reichman has additional training in transgender care and women’s health, and Paula Esteva Slack is certified in gerontology as well as experienced in cardiology and care of patients with complex medical histories. They both also have great enthusiasm for, and growing experience with, a broad range of integrative approaches to primary care.
We are extremely fortunate to also have an acupuncturist, a massage therapist, and a psychotherapist on our team who have many years of experience and longstanding success in their individual practices. We are so lucky to have Abby Humphrey in our clinic. She was a cofounder of the Center for Sacred Healing. She really enjoys collaborating with our physicians in patient care. She provides Traditional Chinese medicine diagnostics and therapeutics, utilizing acupuncture, cupping and TCM herbal blends in her therapy. She provides general care but also has specific expertise in treatment of women’s hormonal issues, long Covid symptoms, aesthetic acupuncture, and anxiety. Prema Smith is a massage therapist well known in the IM community who has expertise in many different modalities including Thai, Swedish, shiatsu, Lomi Lomi as well as neuromuscular massage. Robert Piper is a clinical social worker who uses an integrative approach in his counseling practice, including mindfulness techniques, and hypnosis as indicated.
We are looking for another practitioner to join us. It would be great if we could have a like-minded DO or MD join us who is interested in providing integrative primary care to the general community because there is a shortage of primary care providers, especially independent ones, and we want to provide a supportive place for others who share that goal. But we are definitely open to welcoming other kinds of providers especially nutritionists, manual therapists, and naturopaths.
I would be remiss if I didn’t mention our staff of dedicated administrative assistants, Jessica, Valerie, Suzanne and Kate. They all go above and beyond what is typically expected in their dedication to helping all of our practitioners provide the best and most timely care possible for our patients. They know and care about the patients, they understand the unique aspects of combining high quality allopathic care with other modes of care that may require out of pocket expenses. They work diligently to get patients the information, referrals and clinic visits they need. We could not do what we do without each one of them.
Bill Zirinsky: Dr. Saunders, please tell us how your clinic has fared with Covid over this time? It will soon be three years since the pandemic began?
Dr. Amy Saunders: When the pandemic first started, and schools and businesses shut down we had no idea how long this would last. It seemed like emergency management decisions were needed for what we thought would be a short-term problem. It was an easy business choice to convert our clinic into a remote telemedicine design. My staff and colleagues were very dedicated, and care from home was surprisingly manageable. But then… Covid dragged on and on, with new variants occurring and neither vaccines nor prior illness providing persistent immunity from getting Covid in the future. We have had only a modest number of patients who have rebelled against the CDC guidelines for mask wearing but many people have become frustrated that the measures taken have not successfully ended the pandemic.
We have continued to employ a hybrid patient-care design where each practitioner has some telemedicine days and some in-clinic patient days, and I think that will be an ongoing workable model. In our clinic, it has been required to wear masks ever since the beginning of the pandemic and will continue to be until the prevalence of Covid substantially drops, as it has begun to do. Masks have been quite effective – most people who get Covid have had exposure among family or at indoor events or restaurants where they are unmasked. There have been no cases of Covid among our patients or staff that were caused by exposure at our clinic. That being said, 3-4 of our staff have gotten Covid through exposure in the community or in their homes, and I estimate that 1 of every 4-5 of my patients has had it. The majority of my patients were vaccinated, but among the vaccinated folks who got Covid, most got sick several months after their vaccination. Most have had mild illnesses but a few developed long Covid. We are lucky that Abby Humphrey, the acupuncturist in our clinic, has had good success treating patient with long covid symptoms especially fatigue and brain fog. B vitamins, Vitamin D and C, quercetin, as well as N-acetyl cysteine appear to be helpful in mitigating the effects of Covid.
The incidence of Covid in our clinic is lower than the incidence in Washtenaw County. In Washtenaw County, there have been over 99,700 cases of Covid, and that is likely a substantial underestimation given the home tests that never get reported. The population of the county is 372,000. That does not mean that 1 in 3 or 4 people have gotten Covid, as there are people who have gotten Covid multiple times, but it is probably close.
I am hopeful that the combination of three factors will help us finally turn the corner on this pandemic: the first is the increasing percentage of the population that has either recently been vaccinated or recently been infected. who will be protected from infection for at least 3 months, on average. The second is the new vaccine that is now available for everyone that has improved activity (though not perfect) for the omicron variant. The third is the fact that there have not been new variants galloping across the globe recently, that would lead to a whole new cycle of infection and contagiousness. These factors give us the best chance yet of achieving “herd immunity” – a state where the risk of getting sick – either for the first time or repeated is low -- that it will continue to become less virulent over time. I am looking forward to being able to dine inside at a restaurant sometime this year.
Covid has revealed so much about how our society works. It has helped uncover deep differences we have in opinion about our individual responsibility for helping to maintain the health of the community. While I think the vast majority of people who rebelled against wearing masks and getting vaccinated would be very willing to help a neighbor in distress, many were not willing to acknowledge our role in potentially making others sick. This was especially disheartening early in the pandemic when the hospitalization and death rate were high. Even now, when long Covid can have long term physical, economic and emotional impacts on people, I am discouraged when I hear people dismiss the significance of this illness and the importance for all of us to deal with the consequences of this pandemic.
BZ: Would you share with us about your own journey to Integrative Medicine and how your life experiences brought you there?
Dr. Amy Saunders: I feel in a way that my whole raison d’etre in medicine has been to try to help people by listening to their stories and honoring their own path in seeking to achieve the best health possible for them. My childhood and family trauma history paved the way for that, no doubt. I was left with an early recognition that terrible things happen sometimes and often nobody can say why, and nobody can fix them. But we still must find the best most healthy path through that. In that sense I feel that facing health problems or social problems is our best practice for facing the ultimate “unfixable” issue of our mortality – how do we find our best path when we know that we cannot change that?
My Public Health education gave me a perspective that kept me from getting the myopia that so many doctors have, that the physician is the central character in a person’s healthcare My interest in integrative medicine truly was initially fueled by my recognition that there were so many medical problems that my patients had that we in allopathic medicine were not doing a good enough job providing care for. Chronic musculoskeletal pain, digestive problems, anxiety, insomnia, fatigue, headaches. I thought surely there must be other ways to address these problems beyond the fairly limited number of treatment choices we were taught! When I began to see that musculoskeletal pain was frequently managed much better by PT’s, massage therapists, chiropractors, posture specialists and herbal therapies than by any tools that I had in my doctor bag, that was the thing that began to open my eyes to whole new realms of healthcare.
Once my mind was opened, I chose to apply for the Faculty Scholars Program in Integrative Medicine at University of Michigan. Dr. Sara Warber and Dr. Rita Benn co-created it. The program was designed to bring faculty members from vastly different fields together for a monthly seminar where we learned about different integrative modalities. We met and observed local practitioners. We discussed how the different healthcare paradigms challenged our belief systems, and how what we learned would change how we teach and how we practice in our respective professional fields and our personal lives. I loved the program and working with Rita as well as meeting and collaborating with many integrative providers. I stayed on as co-facilitator for many years. It was life changing for me, and from that point on I have tried to think more broadly about what KINDS of healthcare would be helpful for my patients.
I am not a skilled practitioner of many kinds of integrative treatment modalities, but I have come to appreciate their importance by having an open mind and a modest degree of understanding how various diagnostic and therapeutic processes work. I can feel different kinds of pulses though I am not trained in ayurvedic or Traditional Chinese Medicine. I can sense myofascial restriction and do some simple techniques to relieve that with simple energy work with my hands though I only have a preliminary training in healing touch. I can often detect when patients have somatic dysfunction with malalignment of their pelvis or spine. Though I have only modest training in muscle energy techniques I can often help with the few manual therapies that I have learned. Mostly what I do is act as a “jack of all trades, master of none” who can knowledgeably refer to others who have excellent skills in their field, and also be a bridge for patients, explaining why integrative therapies may be indicated for them.
BZ: At a certain point, you left University of Michigan, and started up your own practice. Please tell us about that?
Dr. Amy Saunders: During my years working at University of Michigan, I learned a tremendous amount working in collaboration with specialists across many disciplines as well as my General Medicine colleagues. The steady salary and the support I got when I had my own health problems were tremendously helpful. But my practice style did not match theirs and I was regularly delinquent in my charting, so I was often in the doghouse. They took away my teaching assignments, which I loved, and did not really help me find solutions for my “dictation block.” I was told I had to leave after working there for 20 years because of my charting problems. I was given retirement, for which I was grateful. And in reality, I was immensely grateful that they pushed me out of that nest, because I don’t think I would have had the courage to do it on my own and truly it was the best thing that could have happened for my career and my life in general. It helped me become the kind of doctor I wanted to be, gave me the courage to embrace more fully a holistic approach to medicine and has allowed me to work with the amazing colleagues I work with today. I have a very good collaborative relationship with my U of M and IHA colleagues – but if I were still working there, I would be unhappy. I worry that the current model of outpatient medical practice – profit-motivated, business-owned, practice algorithm driven, multi-physician employees – is taking us farther and farther away from quality primary care medicine. I think “corporate medicine” is a very apt and sad term for the direction healthcare is going. I rebel against that with every fiber of my being.
Integrative Healthcare providers was established in 2013. I am very happy with our practice philosophy and structure. Our practice provides for personal autonomy for our practitioners in decision-making about how we want our schedule to be – we are all part time – and how much time we feel is best to spend in patient visits. And, of course, we can make nontraditional treatment recommendations that are often just as important as providing the excellent allopathic model of primary care that we do. It also emphasizes the personal autonomy of our patients. In reality, medical care is just one component of each person’s self-care and our role as physicians is to be a consultant, making recommendations and joining the patient as a team to try to achieve the best health possible for them. The idea that patients should be restricted in their healthcare options or personal decision-making is absurd. The lack of open-mindedness in allopathic medicine regarding other treatment paradigms and modalities often, paradoxically, drives patients away from seeking the allopathic medical care they may need.
The struggles I have had running a clinic are in large part what you might expect of any small business. My income is directly related to the number of people we see. The pandemic and the loss of two providers have been financial challenges. But my goal has not been to make as much money as possible and the financial hits have not had destructive effects on our clinic practice. I am lucky that I did not have to be the sole financial provider for my household during the leanest months. I am also lucky that my staff has been committed to staying with our clinic, and flexible throughout the pandemic. Training new staff takes a toll on small businesses, but turnover is lower when all members of a clinic know they are an important member of a team. As a primary care practice there are many ways that “corporate medicine” and government requirements for documentation make things difficult, as well. I am told frequently by my academic colleagues that it is impossible to have a private practice these days and that all individual practices will soon be bought out by healthcare corporations. But I disagree. I also think that the potential for happiness in practicing medicine is greatest in private practice where we have the autonomy to shape our practices the way we want. The research bears this out, as burnout is lowest among physicians in private practice.
BZ: Earlier, you mentioned ‘family trauma history,’ and in the article that Rachel Urist wrote about you for Crazy Wisdom Journal in 2012, you shared some stories. As you look now, how has it impacted your life, and your life’s work? Please do share what you are comfortable with, and what you sense would be illuminating?
Dr. Saunders: I did have many traumatic events happen in my childhood and early adulthood. I went from feeling like one of the luckiest kids on the planet – I was the youngest of six kids in a family that felt secure, with siblings and two parents whom I adored - to having the rug pulled out from under me as family struggles occurred. My mother became mentally ill and then, refusing to take prescribed drugs for it, started drinking, I think to try to self-medicate her demons away. So, she became an alcoholic as well. Conflicts around her illness and poor choices started, and my father left. Then one by one my older siblings went off to college and rarely returned because it was too sad and unfixable. My siblings were my lifeline, and I felt their love, but I was very lonely and felt shame and grief that it has taken me years to acknowledge. I developed a pretty solid veneer, presenting myself in school and with friends as doing just fine.
As we grew into adulthood, my siblings and I lived far apart but remained close. My sister who was 5 years older was especially important in my life. We shared a double bed in a small bedroom until she left for college, and she was more a mother to me than our own for most of my childhood. She was loving, supportive, smart and an inspiration to me. She had polio at age 2 and had residual left arm weakness. She never mentioned it. She excelled in academics and playing the oboe. She became a lawyer and worked for the underserved. When she was diagnosed with advanced breast cancer late in her only pregnancy at age 38 it was devastating. I was in my General Medicine fellowship at the time. I wanted to fix it, brought her to Duke Medical Center for evaluation when I felt the treatment plan, she had was questionable. When metastatic disease was found, she underwent mastectomy and then bone marrow transplant immediately after her daughter was born. I was furious when one of my oncology colleagues said to me, “You know this is just a temporary solution, not a cure.” Hope is a powerful tool for healing, and I did not believe him.
She went through that, and through the depression and fear of having a young baby while unsure whether she would die soon. Then she recovered from the initial treatment and went about living, working, playing, and raising her daughter. She was in remission for 9 years before metastatic disease returned. Nine years when she had a beautiful relationship with her daughter and believed she was cured. She loved people, she appreciated the little miracles of life, rainbows, stories, nature. Then she faced the bad news of her cancer recurrence and further treatments with strength and grace. Then she dealt with the fact that the treatments were not working with the same attitude. She died at age 49.
My brother was just under 2 years older than me, more a playmate than my other siblings. When we reached sixteen, we each started working at Bill Knapp’s restaurant. Part way through college he decided to stop schooling and moved to Palo Alto and became a chef/manager at a restaurant. He was an excellent cook. He decided to go back to school to become a physician after I went to medical school. I think my making it into med school helped him realize that he could do it, too, and that it was his calling. Initially he planned to work in some setting providing care for an underserved population. While in medical school, however, he started to have weakness in his legs. He was diagnosed with chronic progressive multiple sclerosis. He did his residency in Family Medicine, but before the second year was over, he needed a wheelchair. He was not able to do the clinical work of patient care, but he became a leader in the statewide Residents’ Union negotiations in California. Then he went to get a Master’s in Public Health Degree, thinking he could do work that focused on improving access to care. He was not able to work in a job, however, because his health just inexorably worsened. He NEVER complained but stayed involved with friends and the Quaker community. He accepted with grace the ever-increasing need for help from caregivers. He died of MS, also at age 49.
My sister’s capacity to not identify with her illness, and to not dwell on the possibility of a bad outcome, allowed her to focus on and enjoy the beauty in life even with a terminal illness. To the extent I can do that myself and encourage others to do the same, it helps to deal with the frustration of having a chronic illness. Similarly, my brother’s amazing capacity to accept his progressive disability and to “not feel cheated” by what life dealt him is an ongoing source of inspiration to me. I also learned the cliché lesson that bad things happen to good people and that illness is so often unrelated to ‘bad lifestyle choices.’ I have a hard time with people who assume their good health is due to their healthy life choices and they will be guaranteed to stay healthy for as long as they continue with those choices – I especially bristle at the commonly assumed corollary that people who are ill have somehow made lifestyle choices that led to their illness. I will admit to a reflexive anger at that attitude -- that I try to acknowledge in myself -- so it does not negatively impact my caregiving.
The things I learned from my siblings I often share with my patients. Sometimes I recognize it is not fair, as my siblings’ seemingly endless capacity to deal with hardship with grace is unrealistic to expect in people. But I so often see the same strength, resilience, faith, grace, and appreciation of life in my patients who face similarly dreadful diagnoses. In fact, I believe that having to face unwelcome news often strips away some of the simplistic assumptions we have about what our lives “should” be and leads us to reach down inside ourselves to find those reserves of strength and grace that we generally don’t know are there when life is coasting along fine. Two sayings I am apt to quote are “Old age is not for sissies” (because the older my patients get the more likely they are to have had to face these issues due to chronic pain or illness) and the Eleanor Roosevelt quote “women are like tea bags – you never know how strong they are until they get in hot water” -- of course that applies to men as well. I feel truly privileged to have an occupation where I am moved and inspired daily as I am able to witness my patients’ strength and grace, and to partner with them as they navigate the difficult waters of aging and illness.
BZ: And you, yourself, have faced illness and a chronic condition?
Dr. Amy Saunders: Yes. When I got cancer, I was twelve. It was the 60’s when my parents divorced and when I got cancer. Things were vastly different then, in my small hometown. Divorce was not discussed, mental illness was not discussed, cancer was not discussed. There was a strong unspoken message that it was inappropriate to talk about things like that. I remember my eighth grade English teacher called my dad after I chose to speak to the class about my hospital experience for an assignment. She felt it made the kids uncomfortable and asked him to tell me to not talk about it again – and I did not. So, I developed a thicker veneer and more loneliness. And, also, unfortunately, a bit of a martyr complex that it also took me decades to acknowledge. That sense of needing to silence my own story led to my strong conviction that listening to each other’s stories is one of the most powerful healing tools that all of us have.
When I was in the hospital for my cancer surgery, it was the first time I witnessed that strength and the change in perspective that I mentioned that happens when one faces serious illness. I saw it in other kids with cancer in the process of dealing with their illness – and I saw it in me, too. That finding a depth of meaning in life and a recognition of one’s inner resources. I saw it in the doctors and nurses in the hospital, too – they were dealing with grave issues on a daily basis. Both they and the patients were inspiring to me. I think that, as much as my experiences with my dad and his work, were the reasons I decided I wanted to be a caregiver when I grew up.
When I got M.S. at age 38 it was another devastating blow. Having witnessed my brother’s rapid decline and understanding the medical facts of the disease, I was afraid – much more so than when I found I had cancer. (I was too naive at that time to know to be scared.) The journey of trying to find a sense of peace of mind when facing a potentially debilitating disease has been the most important work of my life. I have had a mild course of the disease so different from my brother’s. And, honestly, I cannot credit anything other than good luck as the reason for my mild disease. That has taught me that not just dreadful things happen for no reason, but good things do, too. The importance of recognizing that luck is a major factor in our health is something that I try to convey to patients and students, alike: we do not control as much as we think we do.
BZ: I know that your father was a physician. What influence did he have on you?
Dr. Amy Saunders: I admired my father immensely. He was gentle, smart, and seemed to really enjoy practicing medicine. I would sometimes go with him on rounds at the nursing home or at the clinic. I saw the kindness, warmth, and respect he showed to the staff and to the patients and I saw how they felt the same toward him. Though I never was in an exam room during one of his patient visits, I could tell when they spoke with him in the hallway or when we met them on the street that they felt well cared for. One of the few things that irritated him was when he felt someone was not being treated with respect. A friend and classmate of mine who is Black (an uncommon thing in my hometown, especially in the 60’s) said my dad was the only doctor in town who would make house calls to their house, and that her mother thought highly of him. It is important to me to show the same kind of warmth and respect to patients, staff, and colleagues as he did. He also exuded a sense of calmness as well as a caring demeanor and I aspire to have that calming effect, too, with my patients, though I don’t always achieve it.
BZ: Would you tell us about your medical school training and residency?
Dr. Amy Saunders: My medical training was very Old School in that there was an expectation that once we got on the wards we were basically fully employed as caregivers. By that, I mean feeling a sense of responsibility to our patients – we did not feel like “just learners” at that stage. The teaching was that you never leave the hospital until your patients are stable. That commitment became even more explicit in internship and residency. In a very real sense, it was brutal because the hours were ridiculous. The culture of extreme hard work in clinical medicine was deeply imbedded at Ohio State, where many of our attending physicians would talk about how things were even harder back in their day – ‘the days of the giants’, they would say. While I don’t support that expectation of that kind of overwork at all, I do think there is a benefit to be gained from the immersive experience of intense clinical training. The transition from learner to a physician who feels prepared to make life or death decisions for other people involves not just knowledge but a change in self-image. As a resident we would see the transition happening among the interns often more clearly than we saw it in ourselves. Fortunately, the house staff culture was incredibly supportive, and we all felt like we were in it together. I notice that I am using a lot of expressions that could apply to military or team sports training and there are parallels. I hope with current med school and residency training programs with more reasonable, defined hours and utilization of hospitalists, that there is still an intensive, immersive clinical experience that allows for that internal transition. In this way, it is like any other profession – people we depend on to have deep knowledge about their specialties and a deep commitment to provide top quality work in their careers, as well.
BZ: I know you also wanted to express your thoughts about the Affordable Care Act?
Dr. Amy Saunders: Lastly, about the Affordable Care Act. I have always been a supporter of a single payer, not for profit healthcare system. But a well-regulated private insurance structure as they have in the Netherlands, where everyone is covered and per person costs are controlled and subsidized as needed is also a good design. The ACA intended to have that structure, and I am still a staunch supporter, as millions of people in the US have health insurance that they did not have before. The structure in the US, sadly, is extremely flawed, but I put the blame for that squarely on the Republican Congress who sabotaged it by stripping away the financing as well as the quality assurance components that were in the original bill. Without a modest penalty for those who do not opt in, and without restrictions on health insurance companies on how high they could raise their premiums and deductibles, then it was certainly bound to hit the “already insured” the hardest. Insurance companies are making higher profits than ever - because they are ripping off us consumers and falsely saying the blame is on the ACA. They also should not be allowed to charge high premiums while their cheaper plans have pitiful coverage, and their deductibles are so high that many people never see any benefit. If Congress can continue to rein in insurance and pharmaceutical companies with appropriate regulations on their costs, then the benefit of the ACA may become more appreciated. People who ONLY look at their own pocketbook are ignoring the fact that this has been a lifesaver for so many.
BZ: I understand you became a grandparent not so long ago. How is that going, what are you relishing, what are you noticing?
Dr. Amy Saunders: It sounds so cliche but getting to be a grandparent is one of the greatest joys of my life. I cannot believe I am lucky enough to have my daughter and her family living in Ann Arbor and get to spend time regularly with Ellis. I love the bond we have built. As a grandma, the experience of hanging out together is just less weighty than I often felt as a parent. The silly things are sillier. The worries are less worrisome, the watching him change and learn every day is more delightful. And the other thing that has been an extraordinary joy is to get to see my daughter being a loving mom and my son-in-law be a loving dad. The gift of getting to be an extended family -with my husband, my other daughter, my siblings, my son-in-law’s family all connected- is somehow clearer and more meaningful since my grandchild, a new generation, has arrived.
BZ: What do you love to do in your spare time in the winter, in Ann Arbor and southeastern Michigan?
Dr. Amy Saunders: I enjoy wintertime and the crispness of the air, the smell of the cold. I even find the evening darkness enjoyable especially when there is snow for the lights to reflect off of. During the pandemic we learned how much we enjoy winter walks in the woods. With small woods near us like Scio Woods, Greenview Woods, and meadow, Eberwhite, etc., we have become fairly regular walkers and I love watching and photographing the change of seasons- and winding up at a coffee shop afterwards for a latte. I don’t very often see wildlife during the summer, so it is kind of a kick to see SO many different animal prints in the snow at Scio Woods.
My family and I are great game lover, too, so we often enjoy getting together for dinner, wine, and games.
BZ: Anything else you would like to add?
Dr. Saunders: I would also like to say that I have always felt like I have the best job in the world as a primary care physician. Every day I get to be inspired and learn from and laugh with my patients - at the same time as we deal with a wide variety of health issues that have deep meaning and relevance to each person’s quality of life.
BZ: Thank you!





































Living on a farm in Chelsea, Ramsey’s journey from community developer and social worker to shamanic practitioner and animal chaplain exemplifies an authentic evolution of one’s unfolding of identity, own healing, and epiphany in recognizing one’s place within the actual world contrary to the confines and misperceptions of society.